Medical Education 13: Potpourri
Session: Medical Education 13: Potpourri
276 - My Ideas Matter: Resident Perceptions of the Value Placed on Their Contributions to Patient Care
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 276.5719
Zineb Alfath, University of Minnesota Masonic Children's Hospital, Minneapolis, MN, United States; Rebecca Wiersma, University of Minnesota Masonic Children's Hospital, Minneapolis, MN, United States; Alison Woods, University of Minnesota Masonic Children's Hospital, Minneapolis, MN, United States; Samantha Talerico, Children's Hospitals and Clinics of Minnesota - St. Paul, Minneapolis, MN, United States; Emily Borman-Shoap, University of Minnesota Masonic Children's Hospital, Minneapolis, MN, United States
- ZA
Zineb Alfath, MD (she/her/hers)
Chief Resident
University of Minnesota Masonic Children's Hospital
Minneapolis, Minnesota, United States
Presenting Author(s)
Background: Resident autonomy is an area of significant focus in medical education, but clinical independence is not the only way to promote learner development. The University of Minnesota Pediatric Residency Program's post-rotation surveys not only ask residents to comment on opportunities to exercise autonomy, but also whether they felt that their ideas about patient care were valued and respected.
Objective: The aim of this study is to assess how residents' perceptions of their opportunities for autonomy and of the value placed on their opinions are correlated, and if this varies based on clinical setting or in-house attending presence.
Design/Methods: We reviewed 3228 post-rotation surveys from 2019-2024, focusing on two questions: “on a scale of 1-5, how often did you have the opportunity to exercise your own clinical judgment?” and “on a scale of 1-5, how well did you feel that your ideas about patient care were respected and valued?” Using unpaired t-tests we compared the average scores for rotations based on clinical setting and 24 hour in-house attending presence.
Results: We found statistically significant differences in perceived opportunities to exercise clinical judgment across clinical settings. Subspecialty teams ranked the lowest, followed by the ICU, nursery, and general pediatrics teams, with ED ranking the highest. In the perceived value placed on residents’ ideas about patient care, ICU rotations again ranked lowest, but were followed by nursery, subspecialty teams, and general pediatrics teams. ED again ranked highest. Rotations with attendings in-house 24 hours scored higher than those without for both questions. General pediatrics scored higher than subspecialty rotations on both questions.
Conclusion(s): To understand patterns of learner development, especially with upcoming ACGME changes, it is important to consider how educational factors vary by clinical setting. We found that resident perception of autonomy and whether their ideas were valued did not always correlate. This suggests that even on rotations with limited opportunities for independence, there are ways to help residents feel like their contributions are valuable. Subspecialty teams and ICU rotations scored lower than general pediatrics teams in opportunities to exercise autonomy but did not receive the lowest scores for perceived value placed on residents’ contributions. Conversely, rotations with less attending supervision did not always correlate with residents’ perception of their ideas being respected. This highlights the importance of asking about both autonomy and respect when evaluating clinical training experiences.
Average Scores: "Opportunities to Exercise Clinical Judgment" and "My Ideas About Patient Care were Respected and Valued" Across Clinical Settings
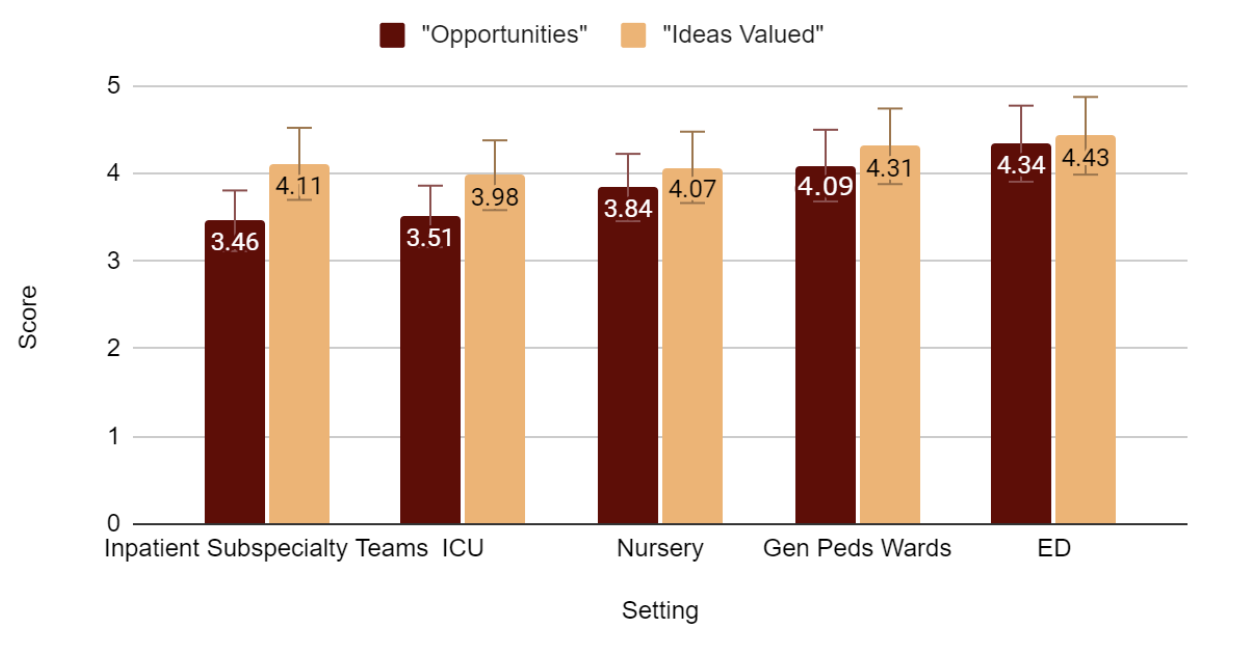 Figure 1: Mean scores for survey questions by general clinical setting encompassing multiple training sites and hospitals. With regards to the question about opportunities to exercise clinical judgment, subspecialty teams ranked the lowest (797 respondents, mean 3.46, +/- 0.68), followed by the ICU (both PICU and NICU, 799 respondents, mean 3.51, +/- 0.77), newborn nursery (79 respondents, mean 3.84, +/- 0.57), general pediatrics teams (1021 respondents, mean 4.09, +/- 0.67), and the ED ranking the highest (532 respondents, mean 4.35 +/- 0.61). With the exception of subspecialty teams, a similar trend was seen in perceived value placed on residents’ ideas about patient care, with ICU rotations ranking lowest (3.98 +/- 0.71), followed by newborn nursery (4.07 +/- 0.59), subspecialty teams (4.11 +/- 0.6), general pediatrics teams (4.31, +/- 0.62), and the ED again ranking the highest (4.43 +/- 0.58).
Figure 1: Mean scores for survey questions by general clinical setting encompassing multiple training sites and hospitals. With regards to the question about opportunities to exercise clinical judgment, subspecialty teams ranked the lowest (797 respondents, mean 3.46, +/- 0.68), followed by the ICU (both PICU and NICU, 799 respondents, mean 3.51, +/- 0.77), newborn nursery (79 respondents, mean 3.84, +/- 0.57), general pediatrics teams (1021 respondents, mean 4.09, +/- 0.67), and the ED ranking the highest (532 respondents, mean 4.35 +/- 0.61). With the exception of subspecialty teams, a similar trend was seen in perceived value placed on residents’ ideas about patient care, with ICU rotations ranking lowest (3.98 +/- 0.71), followed by newborn nursery (4.07 +/- 0.59), subspecialty teams (4.11 +/- 0.6), general pediatrics teams (4.31, +/- 0.62), and the ED again ranking the highest (4.43 +/- 0.58).Average Scores: "Opportunities to Exercise Clinical Judgment" and "My Ideas About Patient Care were Respected and Valued" for General Pediatric vs. Subspecialty Teams
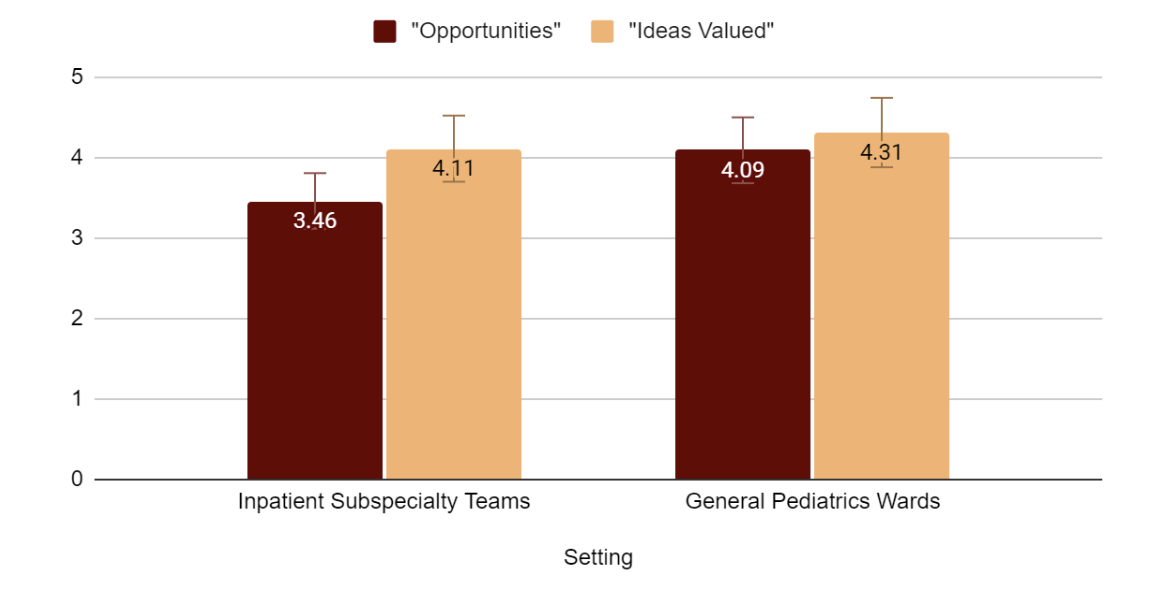 Figure 2: Comparison of general pediatrics wards with subspecialty rotations. With 1,021 respondents, general pediatrics wards scored higher for opportunities to exercise clinical judgment (mean 4.09 +/- 0.67) compared to subspecialty teams with 797 respondents (mean 3.46 +/- 0.68). This was statistically significant (p <0.05). General pediatrics wards also scored higher for perceived value placed on residents’ ideas about patient care, with a mean of 4.31 (+/-0.62) compared to subspecialty teams (4.11 +/-0.6), which was statistically significant (p <0.05).
Figure 2: Comparison of general pediatrics wards with subspecialty rotations. With 1,021 respondents, general pediatrics wards scored higher for opportunities to exercise clinical judgment (mean 4.09 +/- 0.67) compared to subspecialty teams with 797 respondents (mean 3.46 +/- 0.68). This was statistically significant (p <0.05). General pediatrics wards also scored higher for perceived value placed on residents’ ideas about patient care, with a mean of 4.31 (+/-0.62) compared to subspecialty teams (4.11 +/-0.6), which was statistically significant (p <0.05).Average Scores: "Opportunities to Exercise Clinical Judgment" and "My Ideas About Patient Care were Respected and Valued" for Settings with and without 24/7 In-House Attendings
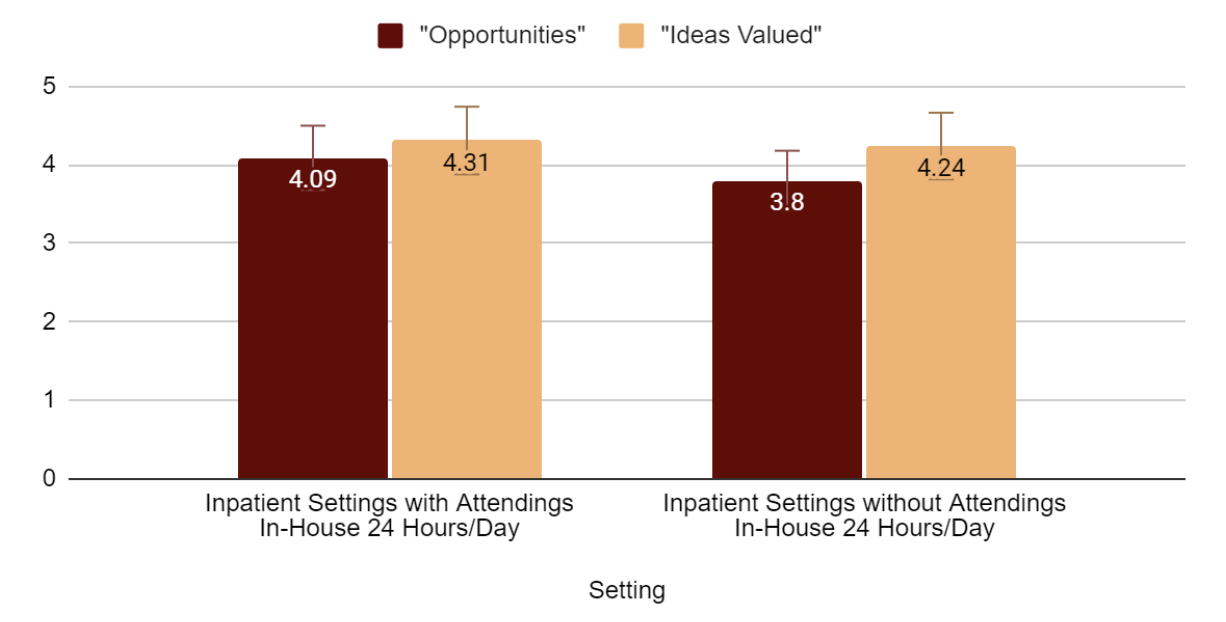 Figure 3: Inpatient wards rotations with attendings in-house 24 hours a day received higher scores (mean 4.09 +/- 0.66) than those without attendings in-house 24 hours a day (3.8 +/- 0.68) for opportunities to exercise clinical judgment, and this was statistically significant (p < 0.05). Wards rotations with attendings in-house 24 hours a day also received higher scores (4.31 +/- 0.6) than those without 24 hour attending presence (4.24 +/- 0.62) for perceived value placed on residents’ ideas about patient care, and this was statistically significant (p <0.05).
Figure 3: Inpatient wards rotations with attendings in-house 24 hours a day received higher scores (mean 4.09 +/- 0.66) than those without attendings in-house 24 hours a day (3.8 +/- 0.68) for opportunities to exercise clinical judgment, and this was statistically significant (p < 0.05). Wards rotations with attendings in-house 24 hours a day also received higher scores (4.31 +/- 0.6) than those without 24 hour attending presence (4.24 +/- 0.62) for perceived value placed on residents’ ideas about patient care, and this was statistically significant (p <0.05). 
