Emergency Medicine 14
Session: Emergency Medicine 14
572 - Magic as an Anxiety-Reducing Tool for Children Undergoing Invasive Procedures in the Emergency Department
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 572.5758
Michelle Khattri, Renaissance School of Medicine at Stony Brook University, Port Jefferson Station, NY, United States; Anne Bennett, Renaissance School of Medicine at Stony Brook University, Port Jefferson, NY, United States; Aaron X. Lopez, Renaissance School of Medicine at Stony Brook University, Great Neck, NY, United States; Anthony J. Sochan, Renaissance School of Medicine at Stony Brook University, Stony Brook, NY, United States; Brandon J. Wong, Stony Brook Children's Hospital, Santa Ana, CA, United States; Anthony Gerald. Chesebro, Renaissance School of Medicine at Stony Brook University, Stony Brook, NY, United States; Harrison D. Pravder, Boston Children's Hospital, Boston, MA, United States; Carl Kaplan, Renaissance School of Medicine at Stony Brook University, Stony Brook, NY, United States

Michelle R. Khattri, BS (she/her/hers)
Medical Student
Renaissance School of Medicine at Stony Brook University
Port Jefferson Station, New York, United States
Presenting Author(s)
Background: Anxiety during invasive procedures in the pediatric emergency department (PED) can cause adverse patient experiences. Varying distraction methods can effectively reduce short-term anxiety in pediatric patients. For example, distraction using magic therapy has shown a 24% anxiety reduction in inpatient units. However, magic as a distraction tool has not been studied in the PED where unique stressors (e.g., time constraints, variable patient load, high acuity) exist.
Objective: To compare provider-delivered magic therapy with established distraction methods from certified child life specialists (CCLS) and expand available non-pharmacological interventions to lower anxiety of children/caregivers in the PED.
Design/Methods: Patients aged 5-16 years undergoing invasive procedures (e.g., needlesticks, COVID swabs, sutures) were randomized into two groups: control (CCLS distractions during procedures) and experimental (magic performed during procedures by medical students trained in MagicAid curriculum). Three evaluation tools assessed child/caregiver anxiety: Visual Analogue Scale (VAS, completed by caregivers and patients, pre- and post-procedure), Faces Pain Scale (FPS, patients, pre- and post-procedure), and Face, Legs, Activity, Cry, and Consolability scale (FLACC, magic therapists, pre- and post-procedure)(Figure 1). Two-sample t-tests were used to compare groups. This study was approved by the Stony Brook University IRB prior to data collection.
Results: 30 subjects (N=19 control) and their caregivers were enrolled. Both groups had comparable anxiety reductions post-procedure with magic and CCLS methods equally effective across all evaluation tools. Caregiver VAS decreased in the control (-14.6, p=0.05) and in the experimental (-29.6, p=0.02) groups. Child VAS also decreased in the control (-22.8, p< 0.01) and in the experimental (-22.1, p=0.03) groups. Additionally, child FPS decreased in the control (-2.9, p=0.01) and in the experimental (-2.6, p=0.06) groups. Lastly, child FLACC decreased in the control (-1.8, p=0.01) and in the experimental (-1.9, p=0.02) groups. There was no significant difference between CCLS distractions and magic therapy (p>0.2 across all groups)(Table 1).
Conclusion(s): Both magic therapy and CCLS standard-of-care significantly reduced child and caregiver anxiety post-procedure. No significant differences were found between the groups, suggesting magic therapy is an equally effective addition to CCLS distractions. Thus, magic can be integrated into the array of interventions aimed at reducing distress in the PED and promoting a positive, interactive experience for patients.
Figure 1. Timeline of Anxiety Assessments and Distractions Used
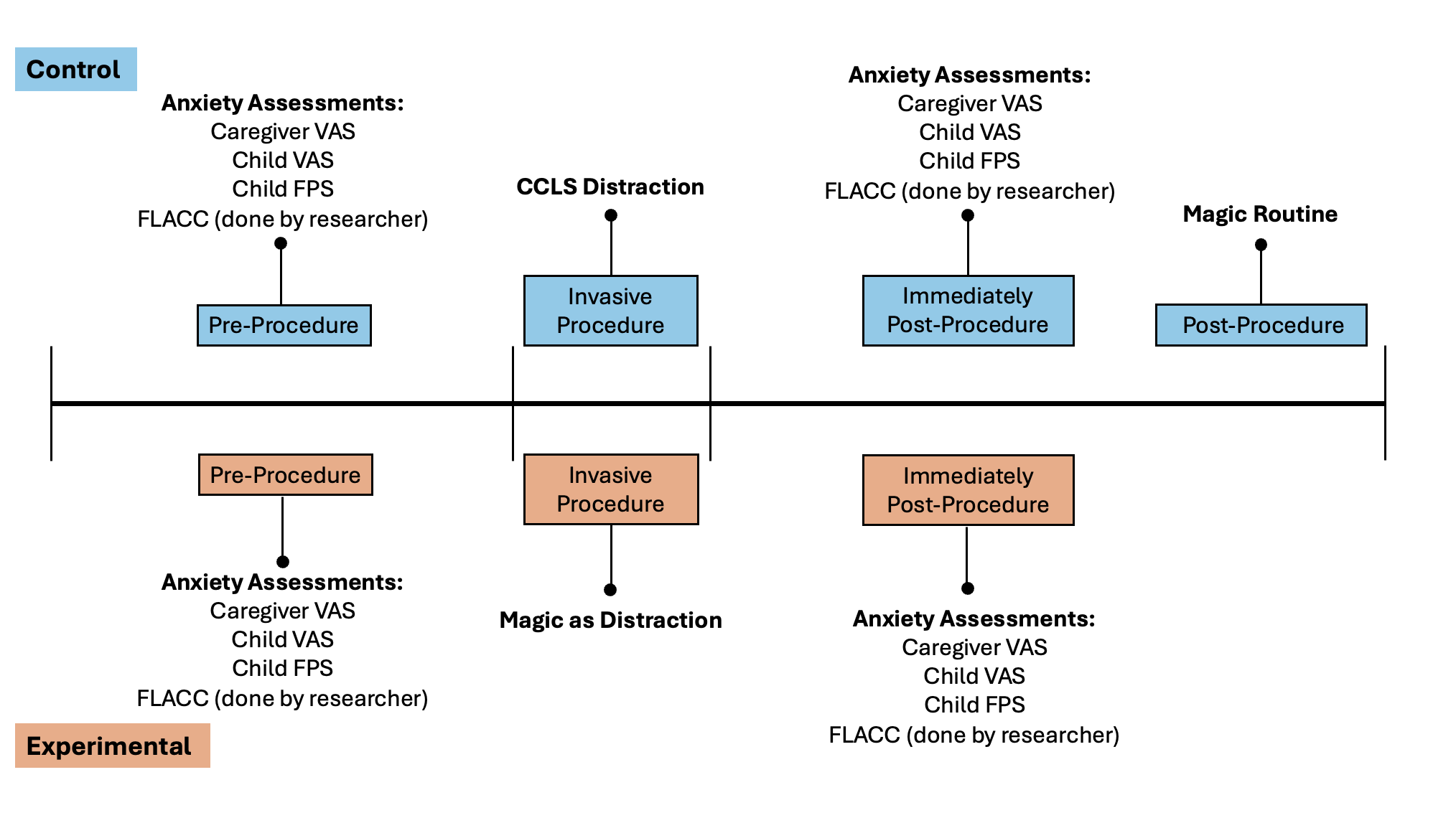 Anxiety assessment tools were completed pre-procedure and again immediately post-procedure. Standard CCLS distractions were done during the invasive procedure for the control group (blue), and magic distraction was done during the invasive procedure for the experimental group (red). A magic routine was still performed for patients in the control group after the needed anxiety metrics were obtained.
Anxiety assessment tools were completed pre-procedure and again immediately post-procedure. Standard CCLS distractions were done during the invasive procedure for the control group (blue), and magic distraction was done during the invasive procedure for the experimental group (red). A magic routine was still performed for patients in the control group after the needed anxiety metrics were obtained.Table 1. Anxiety Scores Pre- and Post-Invasive Procedure for Each Survey
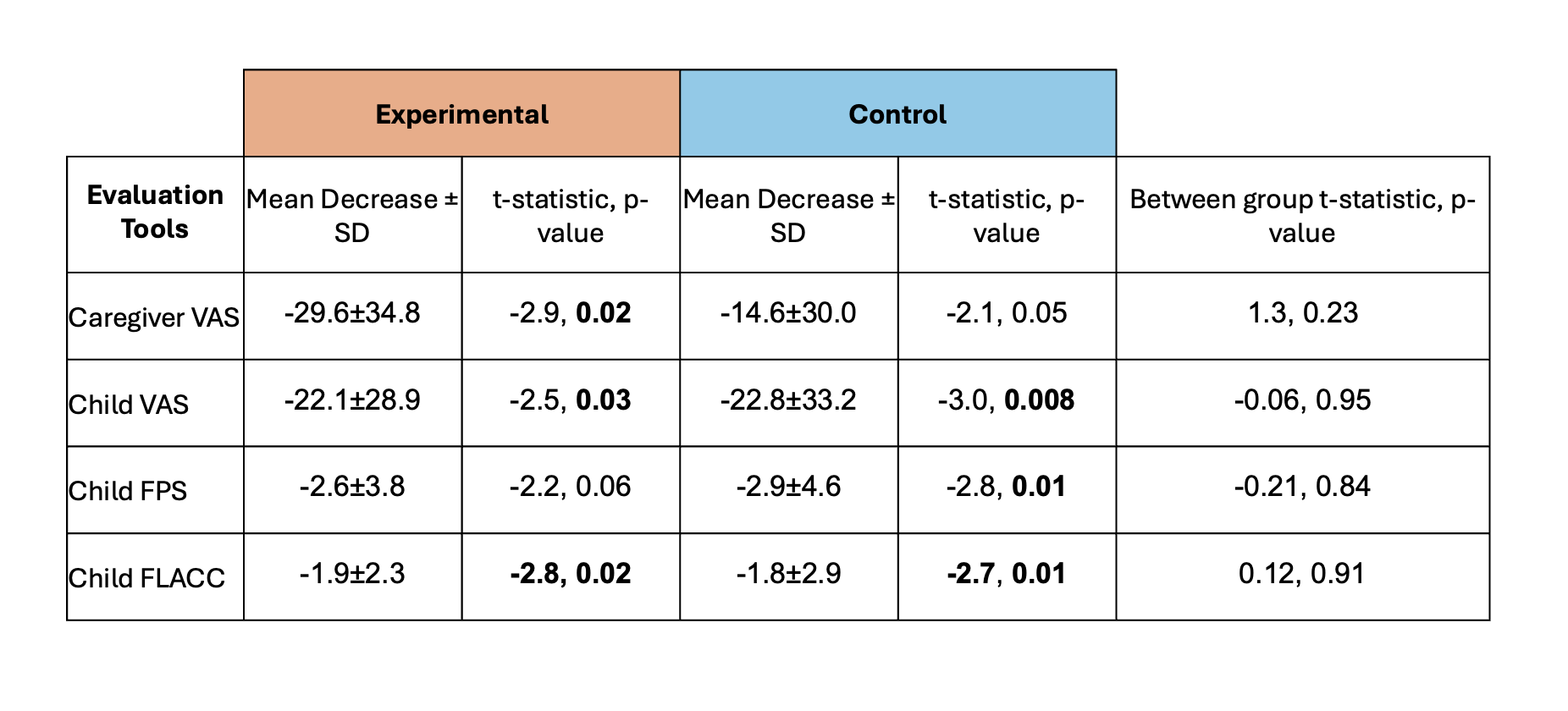 Average anxiety scores for all evaluation tools in both experimental and control groups. Within-group comparisons were assessed by paired two-tailed t-tests; between-group comparisons were assessed by two-sample two-tailed t-tests. P values < 0.05 were considered statistically significant and are highlighted in bold.
Average anxiety scores for all evaluation tools in both experimental and control groups. Within-group comparisons were assessed by paired two-tailed t-tests; between-group comparisons were assessed by two-sample two-tailed t-tests. P values < 0.05 were considered statistically significant and are highlighted in bold.
