Health Equity/Social Determinants of Health 9
Session: Health Equity/Social Determinants of Health 9
182 - Experiences of Past Discrimination Among Black and Latine Caregivers of Hospitalized Children and Communication During Family-Centered-Rounds
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 182.4928
Lauren Wein, Duke University School of Medicine, Rye Brook, NY, United States; Rachel A.. Donaldson, Duke University School of Medicine, Durham, NC, United States; Katie Margolis, Duke University School of Medicine, New Hyde Park, NY, United States; Victoria Parente, Duke University School of Medicine, Durham, NC, United States

Lauren Wein, BA (she/her/hers)
Medical Student
Duke University School of Medicine
Rye Brook, New York, United States
Presenting Author(s)
Background: Experiences of past discrimination (EPD) significantly impact communication between patients and physicians. In adult populations, EPD has been linked to increased demonstration of negative nonverbal expressions, withholding of information, and verbal participation by patients. This phenomenon has not been explored among caregivers of hospitalized pediatric patients during family-centered rounds (FCR), highlighting the need for investigation into how pediatric providers can most effectively engage with caregivers with different experiences.
Objective: To assess the relationship between EPD and caregiver participatory behaviors during FCR.
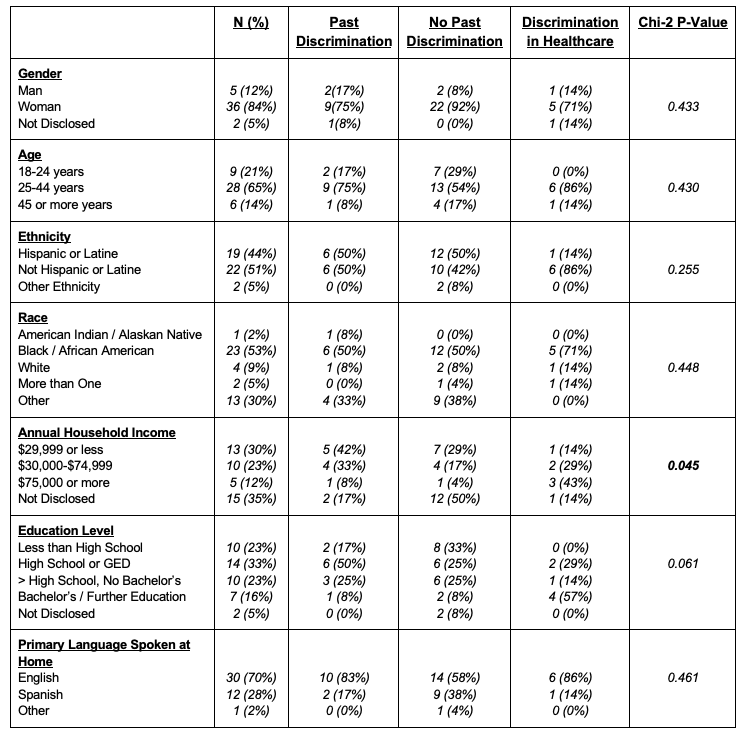
Design/Methods: We conducted a secondary analysis investigating the association between EPD among Black and Latine caregivers and communication on FCR embedded within an equity focused clinician communication intervention trial from 2/2024-7/2024. FCR were recorded and transcribed with caregiver consent, and caregivers completed surveys following FCR. Caregiver surveys collected demographics, ratings of interpersonal processes of care (IPC), and data on EPD. EPD was measured using an abbreviated version of the validated Experiences of Discrimination instrument. We stratified by three caregiver groups: no EPD, EPD in healthcare, and EPD outside healthcare. Caregiver and provider behaviors were double coded by study staff. Chi-squared tests assessed relationships between demographics and EPD. Pairwise Wilcoxon ranksum tests compared caregiver participatory behaviors and caregiver reported communication quality between EPD groups.
Results: We recorded, transcribed, and coded FCR with 43 Black or Latine caregivers; 24 (55.8%) reported no EPD, 12 (27.9%) reported EPD outside of healthcare, and 7 (16.3%) reported EPD in healthcare. Higher income was associated with reported EPD in healthcare, while lower income was associated with reported EPD outside of healthcare (p=0.045). Caregivers with EPD in healthcare asked questions (p=0.02) and made assertive statements (p=0.001) more frequently. Those with EPD outside of healthcare asked questions and made assertive statements less frequently than those with EPD in healthcare and those without EPD. Ratings of IPC did not vary based on EPD.
Conclusion(s): EPD was associated with differences in caregiver participatory behavior on FCR. Approaches to improve communication on rounds must be flexible to account for the impact caregivers’ past experiences, both inside and outside of healthcare, may have on communication.
Caregiver Demographics
EPD and Caregiver Participatory Behaviors / Ratings of IPC
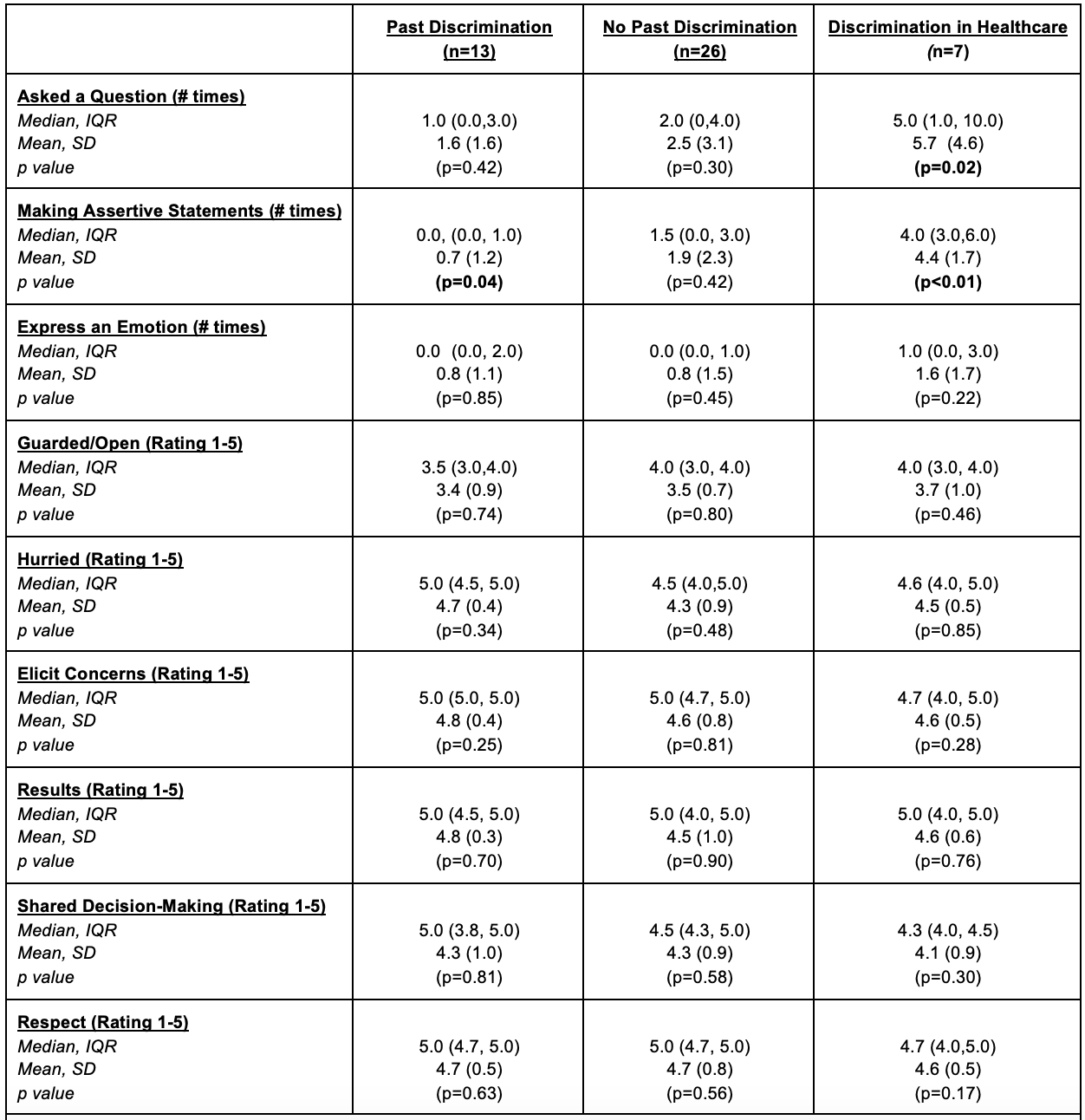 *All wilcoxon ranksum statistics compared each column to the other two columns
*All wilcoxon ranksum statistics compared each column to the other two columns*“Open/Guarded”: global code scores assigned to caregivers by coders (1 guarded to 5 open)
*“Hurried”: scores assigned to providers by caregivers (1 more hurried to 5 less hurried)
*“Elicit Concerns”: scores assigned to providers by caregivers (1 elicited poorly to 5 elicited well)
*”Results”: scores assigned to providers by caregivers based on how providers explained test/exam findings (1 shared poorly to 5 shared well)
*“Shared Decision-Making”: scores assigned to providers by caregivers based on provider practice of shared decision making (1 practiced poorly to 5 practiced well)

