Emergency Medicine 11
Session: Emergency Medicine 11
529 - Equity in Pain Management for Burn Patients Undergoing Debridement at a Regional Pediatric Burn Center
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 529.5004
Brook N. Martell, Childrens Hospital of Michigan, Detroit, MI, United States; Christian Hudson-Bradford, Children's Hospital of Michigan, Ferndale, MI, United States; Ahmad Farooqi, Central Michigan University College of Medicine, Detroit, MI, United States; Kelly Levasseur, Children's Hospital of Michigan, Detroit, MI, United States

Brook N. Martell, DO (she/her/hers)
Fellow
Childrens Hospital of Michigan
Detroit, Michigan, United States
Presenting Author(s)
Background: Effective pain control during burn debridement is crucial for minimizing acute stress disorder (ASD). However, the absence of a standardized pain management protocol for burn debridement can lead to inconsistent practices and potential treatment disparities. This study investigates the presence of racial inequities in pain management among pediatric burn patients.
Objective: The primary objective of this study was to determine if there are inequities in the medical management of pain for those undergoing burn debridement in the pediatric emergency department (PED).
Design/Methods: A retrospective chart review was conducted at a single pediatric burn center, analyzing patients aged 0-18 who received burn-related care in the ED between 2020 and 2023. Eligible patients were identified via the CHM burn registry. Patients who did not have debridement in ED were excluded. Data collected included demographics (race: White, Black, Other), time to medication administration, medication type, and dosage. Total body surface area (BSA) burned was stratified by increments of < 1%, 1%-5%, 5%-10%, and>10 %. Pearson’s Chi-squared test was used to analyze the distribution of categorical variables by groups. Nonparametric Kruskal Wallis test was used to see the difference between the three types of races across the study variables.
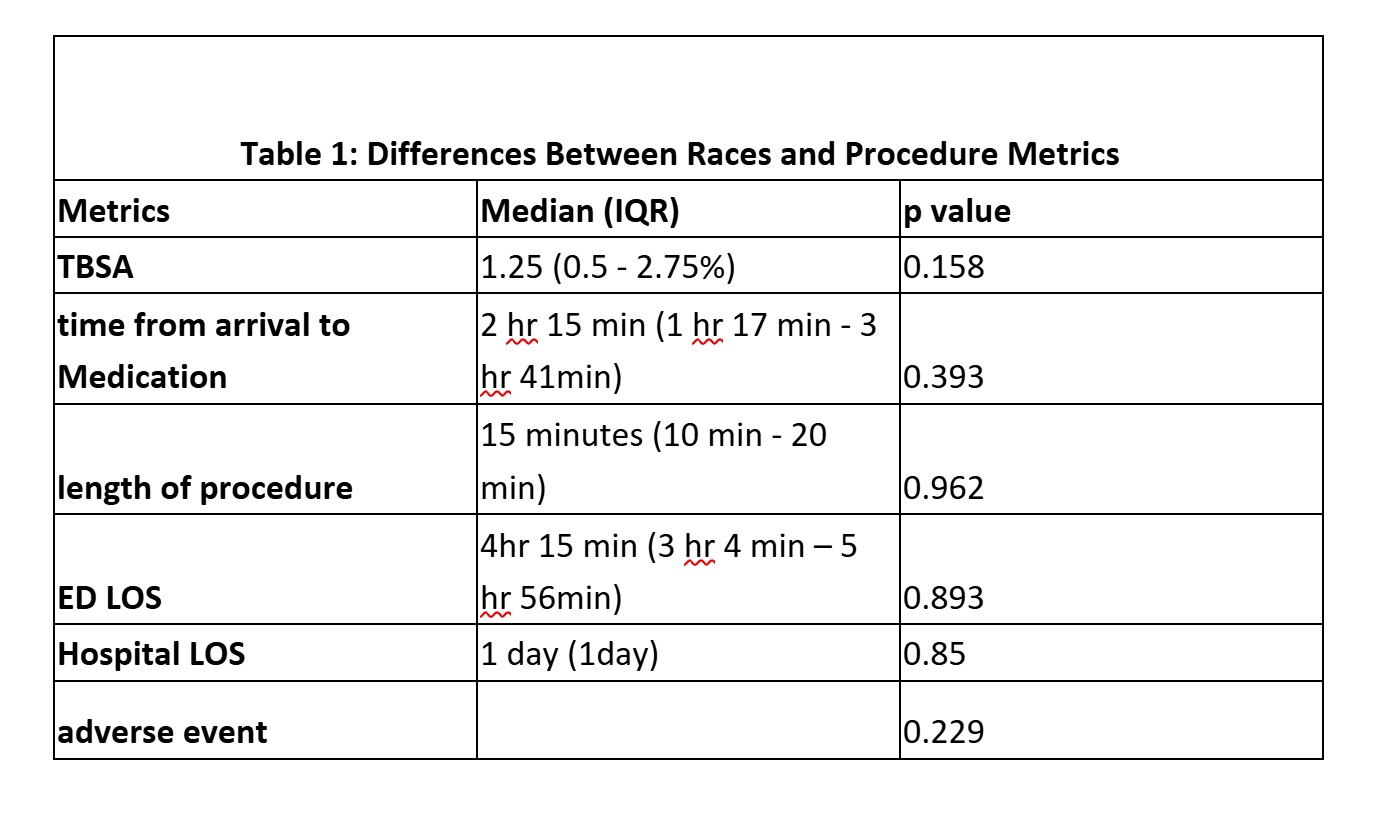
Results: A total of 1356 charts met the inclusion criteria. The majority of patients were male (53%) with a mean age of 9.5 years. 48% of patients identified race as black, 38% as white, and 14% as “other.” The mean TBSA for burn was 3% which did not change based on race (Table 1). No difference was found with TBSA nor the length of the procedure, median of 15 minutes (Table 1). There was no difference in time to sedation based on race nor in length of stay in the ED (median 4 hours and 15 minutes). Finally, no difference was found in adverse events between the three race groups.
Conclusion(s): This study suggests that racial disparities in pain management may not be a significant issue in the context of pediatric burn care at our institution. This is different than other studies looking at time to pain medication in patients with other diagnoses. One reason could be that most of our population is black which could decrease our racial disparities similar to findings of gender disparities when male physicians work with more female physicians. We encourage others to continue to look at disparities in health care and help minimize them in every way possible.
Table 1: Differences Between Races and Procedure Metrics