Children with Chronic Conditions 4
Session: Children with Chronic Conditions 4
476 - Improving Patient and Family Goal Setting in a Pediatric Complex Care Program
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 476.5459
Ryan L. Hubbell, Medical College of Wisconsin, Milwaukee, WI, United States; Jessica L.. Schnell, Medical College of Wisconsin, Milwaukee, WI, United States
.jpeg.jpg)
Ryan L. Hubbell, BS (he/him/his)
Medical Student
Medical College of Wisconsin
Milwaukee, Wisconsin, United States
Presenting Author(s)
Background: Complex Care Programs (CCP) provide medical co-management and care coordination services for children with medical complexity (CMC). Patient and family goals are an important part of CCP clinic visits, as they influence the shared decision-making process by identifying family priorities and expectations. Goals also help focus CCP efforts toward what families value most. The Children’s WI CCP is held accountable for family goal-setting performance through yearly external audits. In 2022 the audit noted only 8% of documented goals met criteria for actionable items and timeframes. This project aims to enhance care provided by the CCP by improving the goal-setting process.
Objective: To improve the percentage of family goals discussed during CCP clinic visits that are actionable and timebound from baseline to a goal of 70% within 12 months.
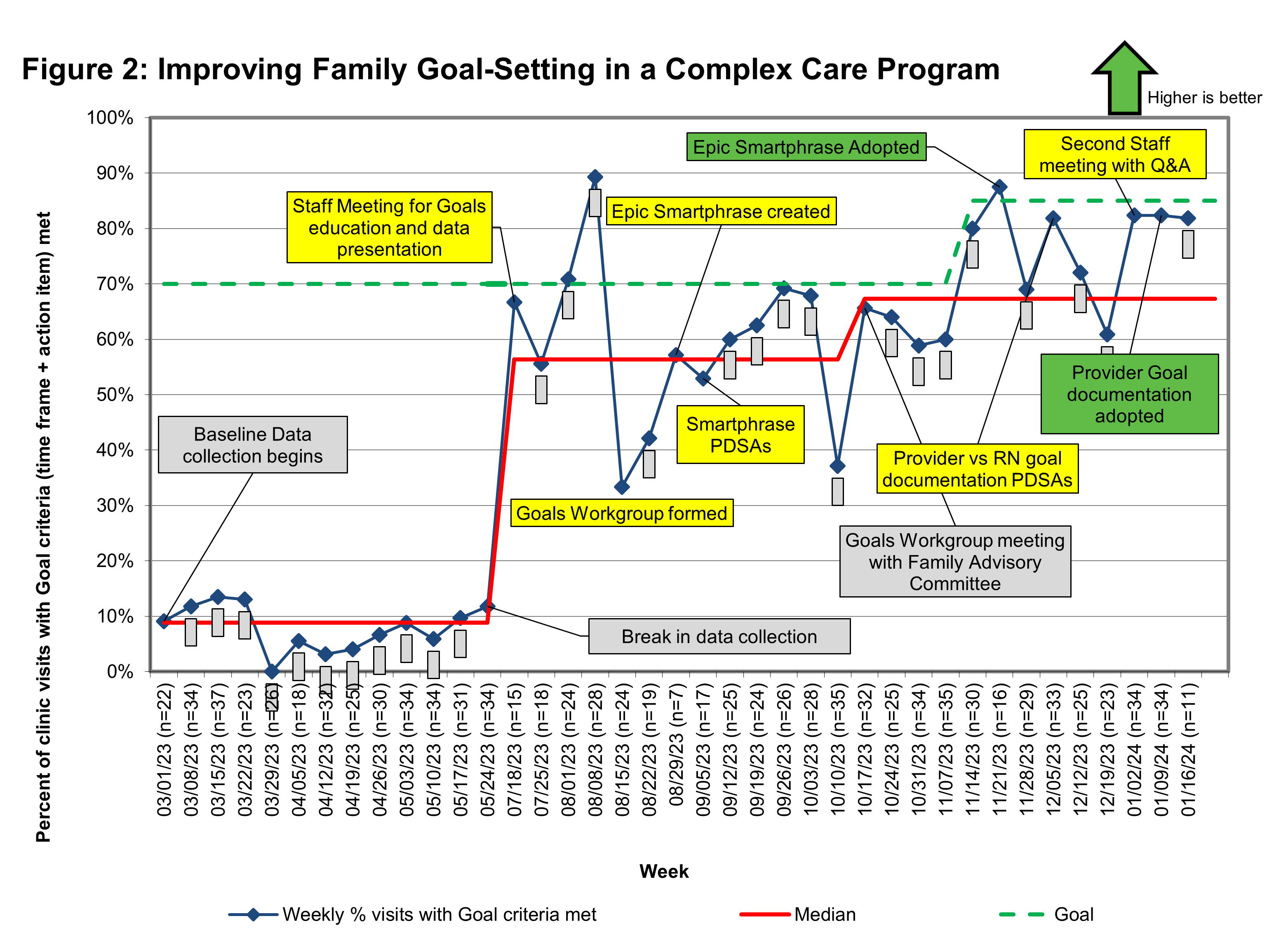
Design/Methods: Baseline data were collected via observation of goal-setting conversations and retrospective chart review of all CCP clinic visits from 3/1-5/31/23. Information collected included details of goal discussion, documentation, and whether audit criteria were met. A key driver diagram (Fig. 1) identified areas for potential improvement. Interventions were developed and tested using PDSA cycles. Interventions included staff education and implementation of documentation and workflow changes led by an interdisciplinary staff workgroup. Ongoing data were collected using prospective chart review.
Results: All 350 baseline visits included a goal-setting discussion, 66% discussed action steps, 13% discussed a time frame of attaining at least one goal, and only 31/348 (9%) of visits met both criteria. Barriers identified included a misunderstanding of criteria, variable documentation location, and poorly-defined staff roles and responsibilities for the goal-setting conversation, and anticipated negative family reactions. Interventions and weekly data were tracked using a run chart (Fig. 2). After interventions, 82% of visits met both criteria.
Conclusion(s): Interventions improved the goal-setting process and were well-received by staff and families. A workgroup including representation from all staff roles helped address barriers and implemented PDSA cycles. The workgroup met with the CCP’s family advisory committee to discuss family perception of the goal-setting process which provided particularly meaningful qualitative data for staff, fostering high uptake of interventions. Ongoing work includes gathering feedback from families and staff.
Figure 1: Key Driver Diagram
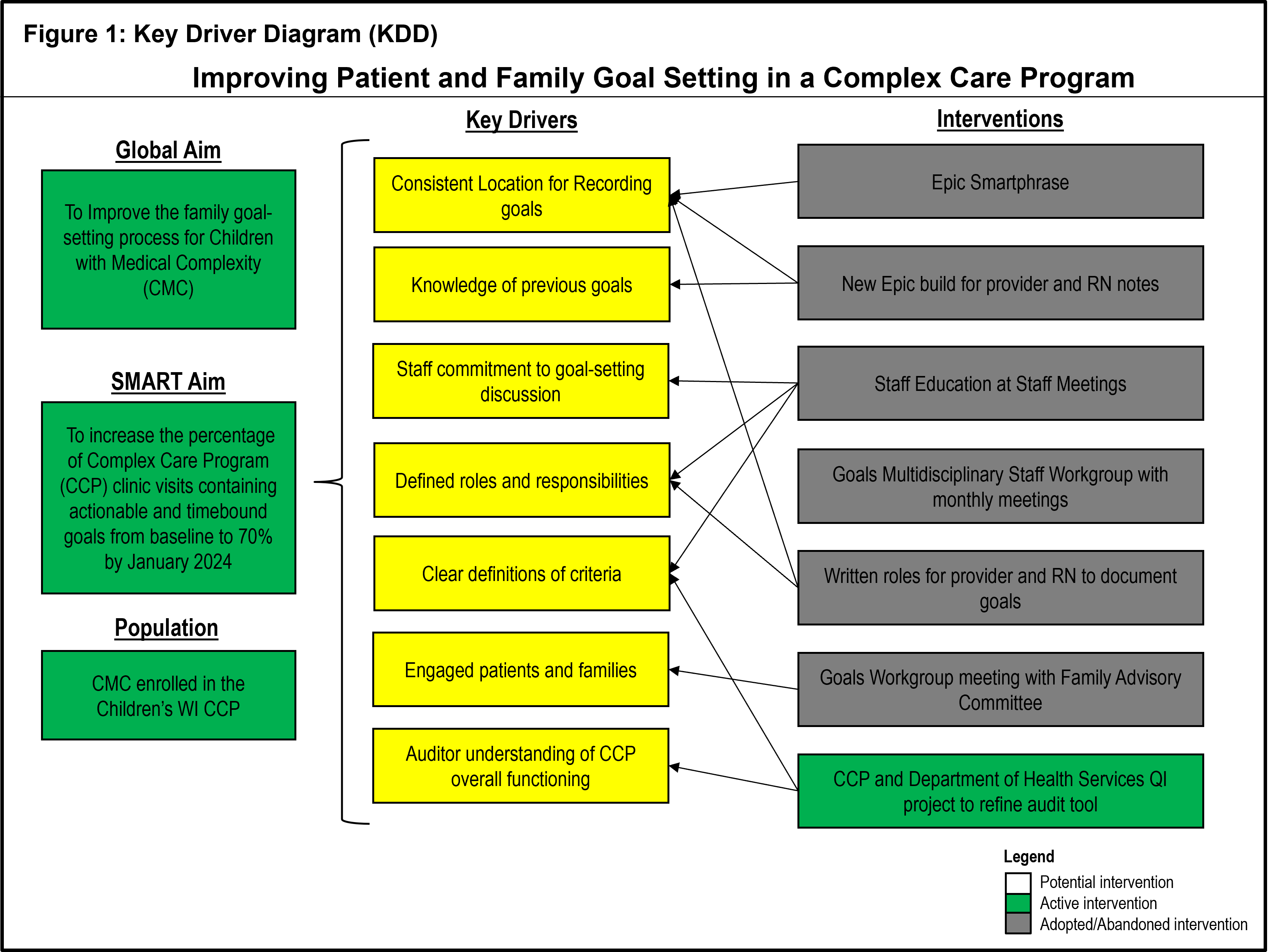
Figure 2: Run Chart