Emergency Medicine 13
Session: Emergency Medicine 13
555 - Hidden in Plain Sight: Identifying Occult Intimate Partner Violence in the Emergency Department
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 555.5470
Monique Huertas, Yale-New Haven Children's Hospital, New Haven, CT, United States; Nishah Jaferi, Yale School of Medicine, Boca Raton, FL, United States; Rebecka May. Hoffman, Yale School of Medicine, New Haven, CT, United States; Caitlin R. Ryus, Yale School of Medicine, New Haven, CT, United States; Gunjan Tiyyagura, Yale School of Medicine, New Haven, CT, United States

Monique M. Huertas, MD (she/her/hers)
PGY-3
Yale-New Haven Children's Hospital
New Haven, Connecticut, United States
Presenting Author(s)
Background: Intimate partner violence (IPV) affects 1 in 4 U.S. women, with 15.5 million children exposed annually. Victims often visit emergency departments (EDs) for diverse health issues, often without disclosing abuse or showing obvious trauma. Despite national recommendations for universal IPV screening, randomized trials show no significant reduction in IPV or improvement in quality of life between screened and non-screened patients. The effectiveness of screening in detecting occult IPV—cases not primarily related to IPV—remains unclear, prompting investigation into nurse-initiated screening for these hidden cases.
Objective: This study aims to evaluate how frequently nurse-initiated screening identifies occult IPV in one ED and to describe the ED interventions provided for identified IPV victims.
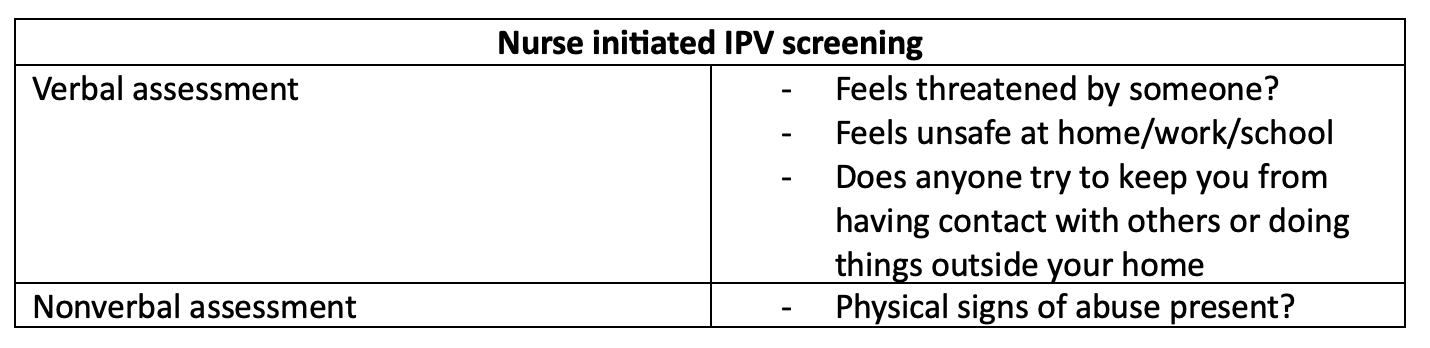
Design/Methods: We conducted a secondary analysis of a retrospective study of patients presenting to a tertiary ED before (June 1–Aug 31, 2019) and after (June 1–Aug 31, 2020) COVID-19 visitor restrictions. The primary study reviewed nurse-initiated IPV screenings (Table 1) and positive screen rates. Cases with positive responses on four IPV screening questions were included, classified as occult if the complaint was unrelated to IPV and disclosure occurred with a provider or social worker, not at triage. Data on social work involvement, IPV resource provision, and police or CPS involvement were collected.
Results: Among 17,559 ED encounters, nurse-initiated screening identified 459 (2.6%) positive cases, with 96 (0.5%) confirmed as true IPV. Of these, 30 (0.2%) were classified as occult and 66 (0.3%) as non-occult. Occult disclosures occurred with healthcare providers or social workers, while non-occult cases disclosed at triage. Social work consults were performed in 93% of occult and 85% of non-occult cases, with resource provision lower in occult cases (57% vs. 77%, p=0.388). Resource provision was consistent across gender, race, and age. Police involvement was higher in non-occult cases (50% vs. 13%, p=0.0014). In cases involving minors under 18, all 13 non-occult cases resulted in CPS referrals, while no children were present in the occult cases.
Conclusion(s): Nurse-initiated universal screening found very few cases of occult IPV in the ED. These findings provide further evidence that universal screening may not lead to adequate detection of IPV in ED settings. No significant differences were found in resource provision between occult and non-occult cases, which may reflect a type 2 error due to the small sample size. These results highlight the need for an improved system to support survivors of IPV within EDs.
Nurse Initiated IPV Screening Questions