Emergency Medicine 13
Session: Emergency Medicine 13
557 - Introduction of a Checklist to Standardize Pre-Procedural Sedation Timeout
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 557.5108
Sujung Kim, Rady Children's Hospital San Diego, San Diego, CA, United States; Karen Yaphockun, Rady Children's Hospital San Diego/UCSD, San Diego, CA, United States; Daniel Roderick, Rady Children's Hospital San Diego, San Diego, CA, United States; Jillian Berman, Rady Children's Hospital San Diego, San Diego, CA, United States; Amy Bryl, Rady Children's Hospital/University of California San Diego, San Diego, CA, United States; Elise Zimmerman, Rady Children’s Hospital- UCSD, San Diego, CA, United States

Sujung Kim, MD (she/her/hers)
Fellow
Rady Children's Hospital San Diego
San Diego, California, United States
Presenting Author(s)
Background: Sedations are routinely conducted in the pediatric emergency department (ED), with ketamine being one of the most commonly used agents. While effective, ketamine administration can lead to adverse events, such as laryngospasm, respiratory depression or apnea, and emesis. In our ED, we experienced a sentinel event during a ketamine sedation, in which a patient experienced laryngospasm and cardiac arrest, requiring cardiopulmonary resuscitation. A root cause analysis identified improper equipment setup. Thereby, we identified the need for a standardized pre-procedural sedation checklist to ensure proper equipment preparation to prevent sentinel events.
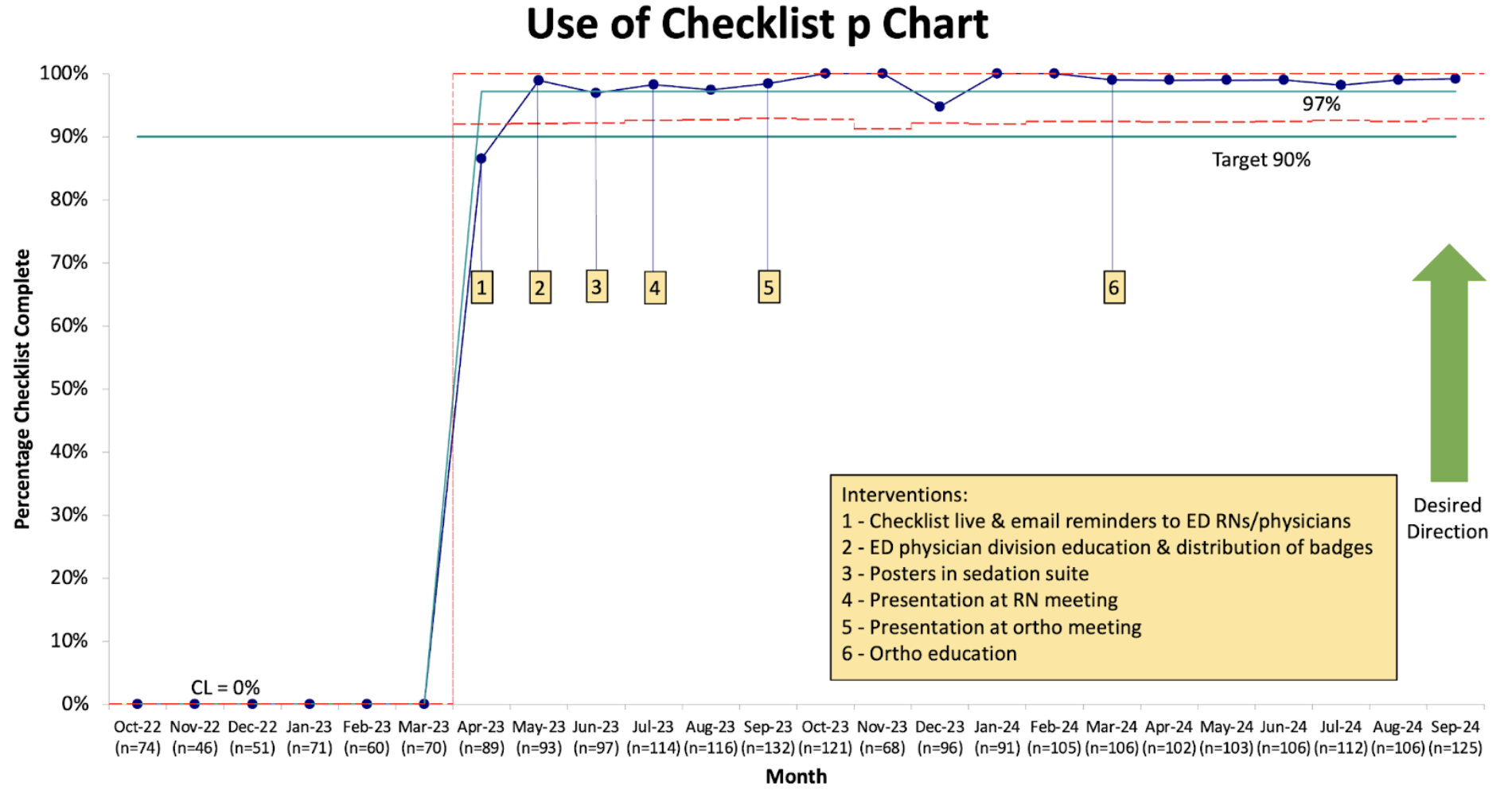
Objective: The primary aim of this study was to increase the utilization of a pre-procedural sedation checklist in the pediatric ED (PED) from 0% to 90% over 12 months.
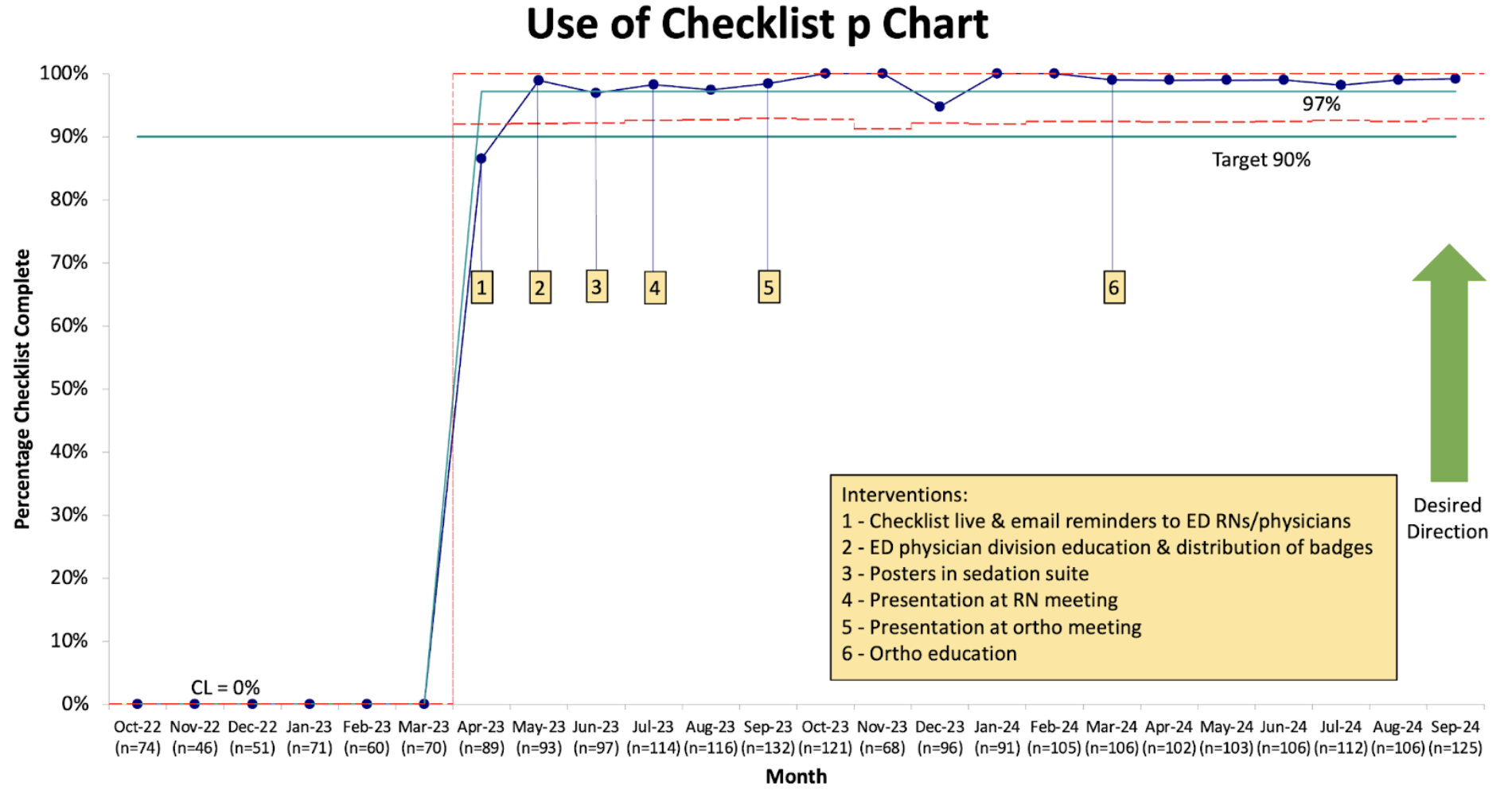
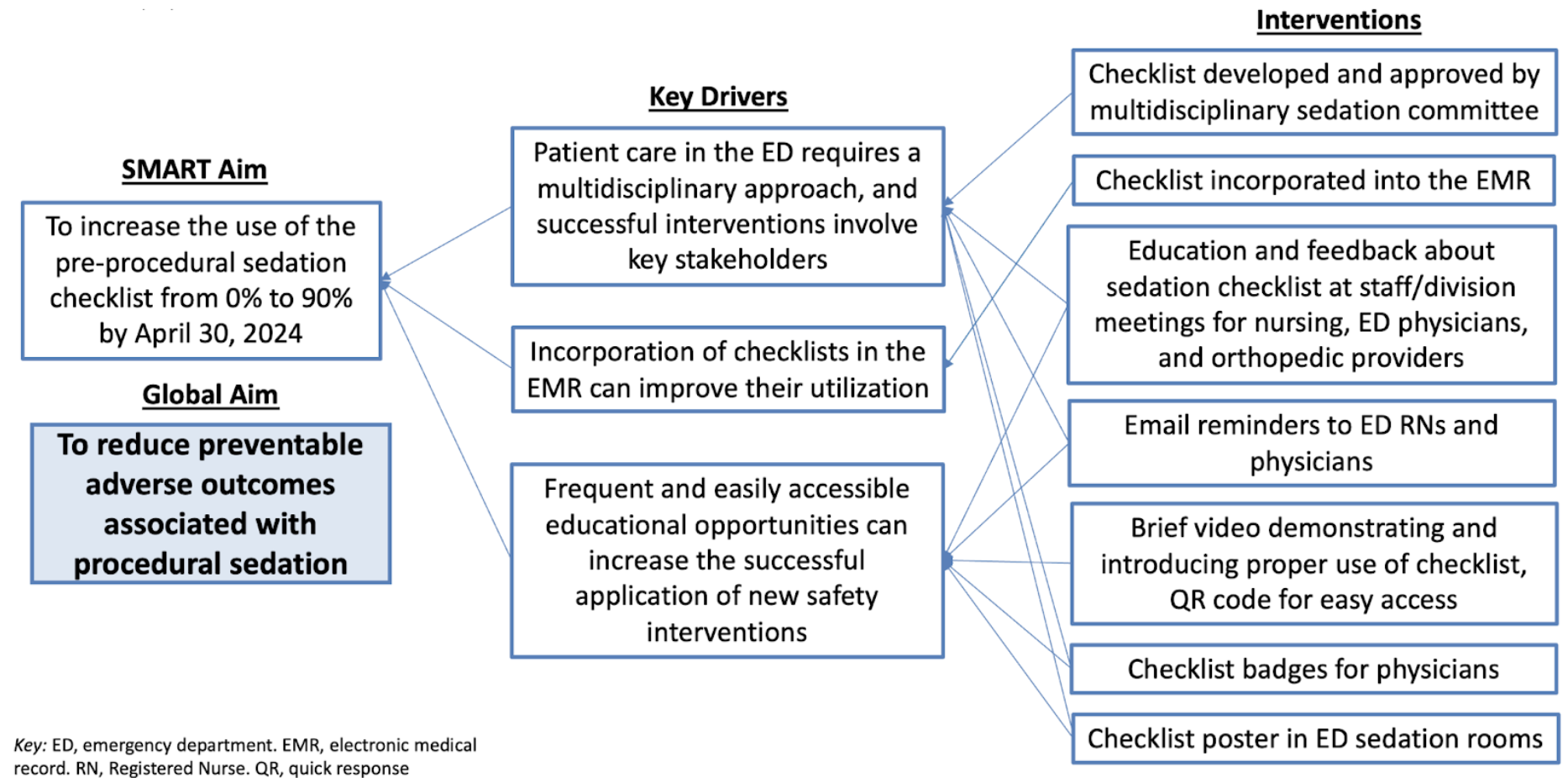
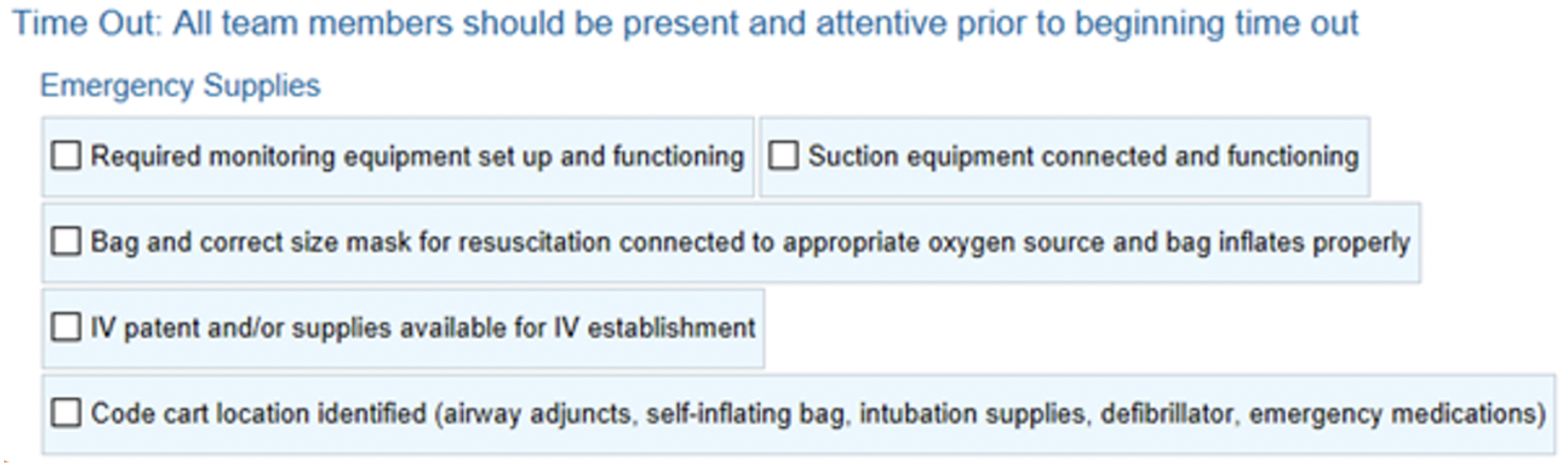
Design/Methods: A multidisciplinary team comprising ED physicians, anesthesiologists, and nurses created a pre-sedation checklist. This was approved for implementation in the ED and hospital-wide. A key driver diagram was created to identify critical drivers and interventions to sedation checklist use (Figure 1). The checklist was embedded into our electronic medical record (EMR) system (Figure 2). Plan-Do-Study-Act cycles were performed, with educational interventions including division and staff meeting presentations and feedback, email reminders, creation of a brief educational video accessible via Quick Response (QR) code, development of checklist badges, and a poster displayed in the sedation rooms of the ED. We used statistical process control to examine changes in measures over time. The outcome measure was the number of sedations conducted since the last sentinel event, defined by the need for intubation, cardiopulmonary resuscitation, neuromuscular blockade, or unplanned hospitalization. Balancing measures included duration of sedation and ED length of stay (LOS).
Results: The use of the standardized sedation checklist increased from 0% to 97% (Figure 3). Post-implementation, no sedation-related sentinel events were recorded. To date, there have been 2,249 sedations since the last sentinel event. The duration of sedation did increase from a CL of 39 minutes to 44 minutes (UCL 50, LCL 38). However, the ED LOS for sedated patients did not change, remaining at a CL of 386 minutes (UCL 442, LCL 331).
Conclusion(s): Introducing a standardized pre-sedation checklist enhanced the safety of ED procedural sedations without affecting ED LOS. Integrating the checklist into the EMR proved to be the most effective intervention.
Key Driver Diagram
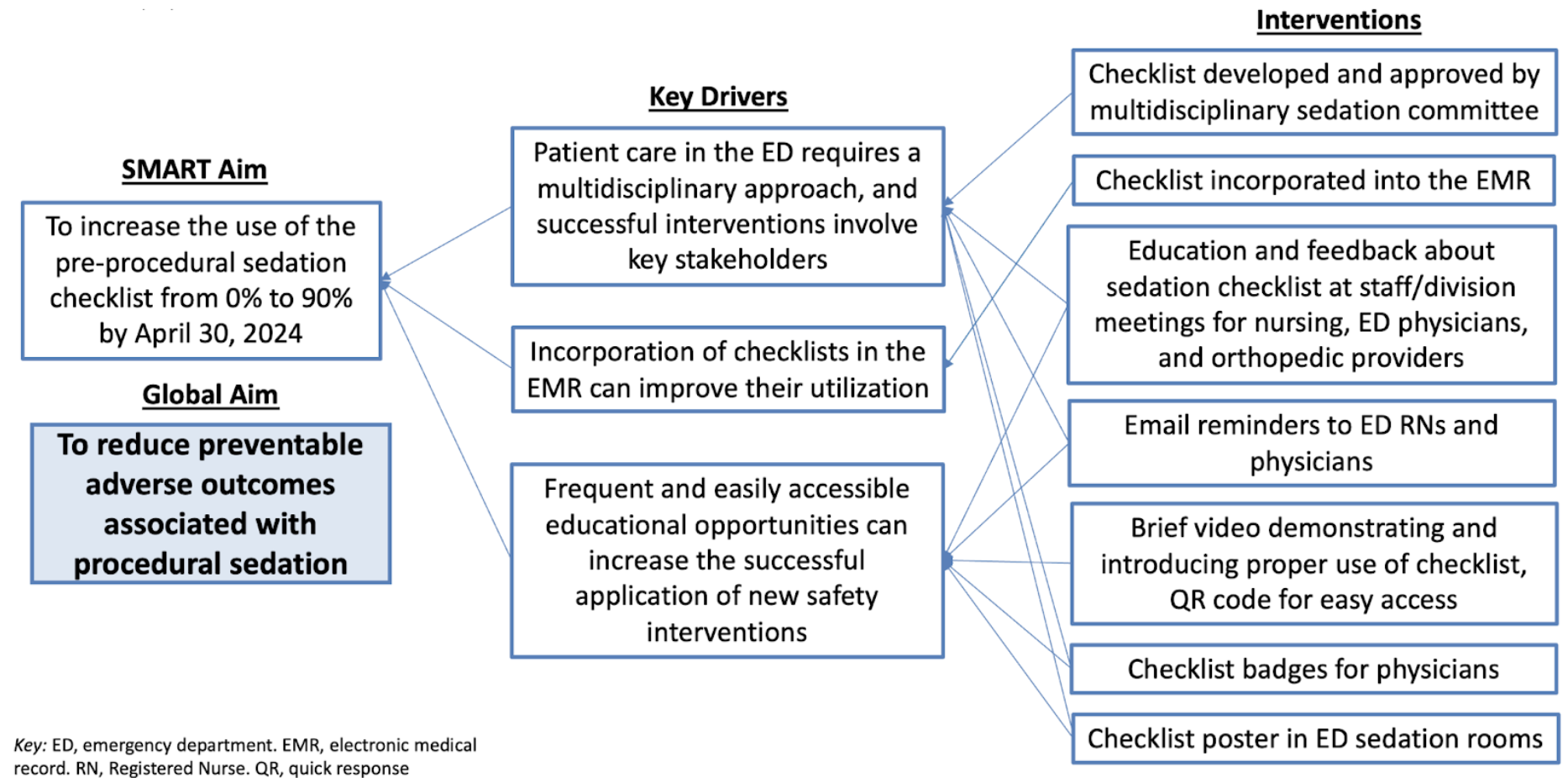
Sedation Checklist in EMR
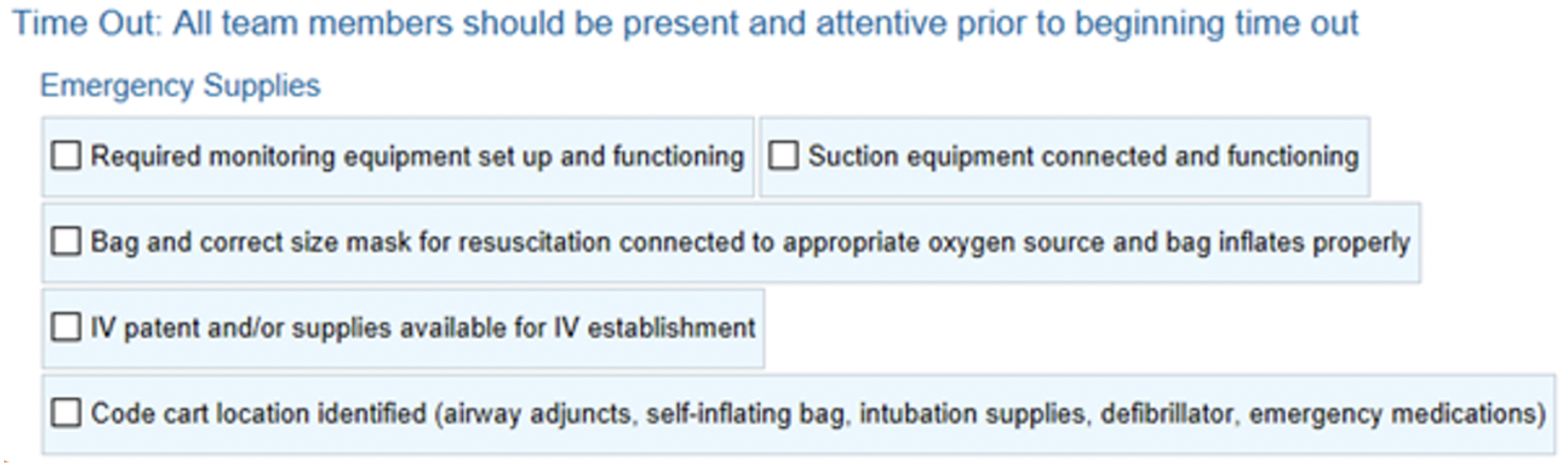
Use of Checklist P Chart
Key Driver Diagram
Sedation Checklist in EMR
Use of Checklist P Chart