Adolescent Medicine 4: Hot Topics
Session: Adolescent Medicine 4: Hot Topics
121 - “I Just Knew That I Needed Help”: Adolescents Speak about Medication Treatment for Opioid Use Disorder in the Fentanyl Era
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 121.3754
Catherine Raney, Ravenswood Family Health Network, Palo Alto, CA, United States; Julia H. Raney, Stanford University School of Medicine, Palo Alto, CA, United States; Janine Bruce, Stanford University School of Medicine, Stanford, CA, United States; Paige Tripp, University of California, San Francisco, School of Medicine, San Francisco, CA, United States; Bonnie Halpern-Felsher, Stanford University School of Medicine, Palo Alto, CA, United States; Lee AA. Trope, Santa Clara Valley Medical Center, Berkeley, CA, United States; Jayme Congdon, University of California, San Francisco, School of Medicine, San Francisco, CA, United States
- CR
Catherine Raney, MD (she/her/hers)
Primary Care Pediatrician
Ravenswood Family Health Network
Palo Alto, California, United States
Presenting Author(s)
Background: Overdose deaths, of which opioids cause 90%, are the third leading cause of death in adolescents and young adults (AYAs). While medication treatment for OUD (MOUD), namely buprenorphine, has been shown to reduce AYA overdose, few AYAs receive timely access. Additionally, there are significant disparities in access to MOUD based on race, ethnicity, gender, and age. Little is known about AYA experiences with starting and continuing MOUD, which is critical to designing equitable, patient-centered programs.
Objective: To investigate facilitators, barriers, and health services preferences related to MOUD among AYAs desiring treatment for OUD within a safety net health system.
Design/Methods: We conducted 11 semi-structured qualitative interviews with patients aged 16-21 who recently initiated MOUD in a county safety-net health system. Patients started MOUD (primarily buprenorphine) in inpatient, outpatient/home, and emergency department settings. The Capability, Opportunity, and Motivation Model of Behavior (COM-B) framework informed interview guides and qualitative analysis. We employed combined inductive and deductive coding and thematic analysis.
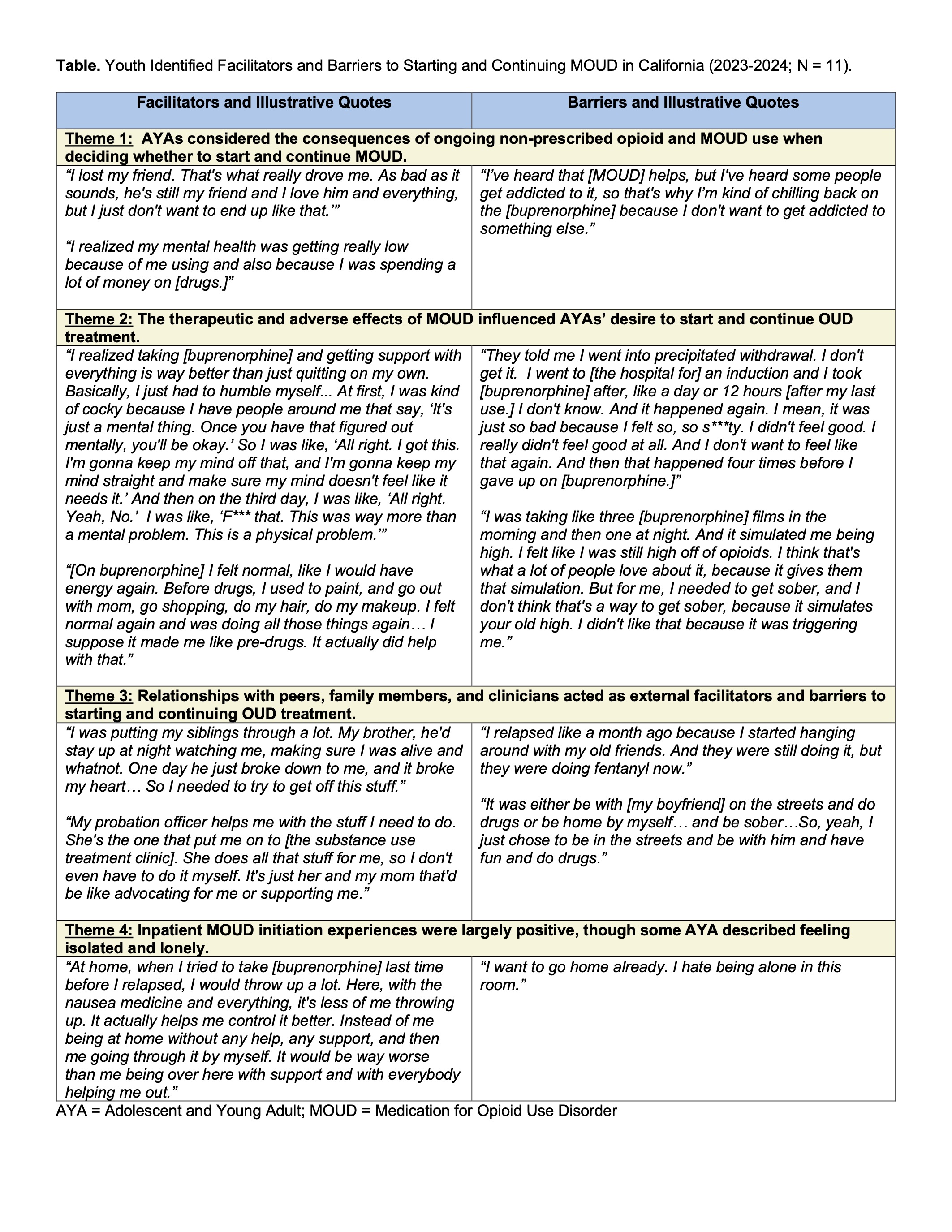
Results: Ten of 11 (91%) AYAs identified as Latine and 9 (82%) were publicly insured. We identified four themes: 1) AYAs considered the consequences of ongoing non-prescribed opioid and MOUD use when deciding whether to start and continue MOUD. 2) The therapeutic and adverse effects of MOUD influenced AYAs’ desire to start and continue OUD treatment. 3) Relationships with peers, family members, and clinicians acted as external facilitators and barriers to starting and continuing OUD treatment. 4) Inpatient MOUD initiation experiences were largely positive, though some AYA described feeling isolated and lonely.
Conclusion(s): Participants shared motivating factors and internal and external barriers to starting and continuing MOUD, and that they appreciated flexible and supportive treatment options, including the opportunity to start buprenorphine inpatient. AYA perspectives such as these can provide essential input into future larger-scale research and clinical and public health programs to improve urgently needed MOUD treatment in this population.
Table. Youth Identified Facilitators and Barriers to Starting and Continuing MOUD in California (2023-2024; N = 11).