Children with Chronic Conditions 4
Session: Children with Chronic Conditions 4
473 - Do I Really Need to Know This? Pediatric Residents' Self Reported Perceived Relevance of Caring for CMC to Future Careers
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 473.4063
Elizabeth A. Hill, University of Utah School of Medicine, Salt Lake City, UT, United States; Nancy A. Murphy, University of Utah Health Sciences Center, Salt Lake City, UT, United States; Laura Murphy, University of Utah School of Medicine, Salt Lake City, UT, United States; Alyssa Kreutzjans, University of Utah School of Medicine, Cottonwood Heights, UT, United States; Stefanie G. Ames, University of Utah School of Medicine, Salt Lake City, UT, United States; Kathleen Huth, Boston Children's Hospital / Harvard Medical School, Boston, MA, United States

Elizabeth A. Hill, DO (she/her/hers)
Assistant Professor
University of Utah School of Medicine
Salt Lake City, Utah, United States
Presenting Author(s)
Background: Children with medical complexity (CMC) have multisystem conditions, high medical fragility, technology dependence, functional limitations, and frequent healthcare interactions. Despite frequent encounters with CMC in the healthcare system, pediatric residents’ exposure to clinical training to meet competency in caring for CMC is limited. Prior research shows gaps in pediatric residents’ confidence in care of CMC. However, it is unknown how relevant residents perceive this training to be to their future careers.
Objective: To describe residents’ self-reported perceptions of the relevance of activities required to care for CMC to their future careers by duration of training and planned career path.
Design/Methods: This is a cross-sectional survey study including residents (post graduate year (PGY) 1-5) in a moderately sized pediatric academic residency program. Residents were anonymously surveyed on future career plans, prior experience with CMC before medical training, self-entrustment in key clinical activities in complex care, and perceived relevance to their future careers. Responses from individual participants were analyzed using a composite score for relevance for standardization and observing overall trends. Descriptive and univariate comparison statistics were performed.
Results: Of the 110 residents invited, 88 (80%) completed the survey. Participants were distributed across all PGYs (1-5) including categorical pediatrics (73%), med peds (6%), pediatric neurology (6%), peds psychiatry (15%), and genetics (1%). Career plans included subspecialty pediatrics (n=28, 32%) and outpatient general pediatrics (n=24, 27%). Only few participants had any prior experience with CMC (n=8, 9%). The mean perceived relevance for all residents was 46(±13)/70 and relevance decreased as years of training increased (p=0.04) (Fig 1). In addition, perceived relevance varied by planned future career (p=0.002) (Fig 2). Pediatric residents pursuing hospitalist medicine report the highest relevance to future career in these key clinical activities.
Conclusion(s): Pediatric residents self-report decreasing perceived relevance of activities required to care for CMC to their future careers as PGY increased. This is concerning for the growing population of CMC who need a well prepared workforce to care for them. Further research is needed to determine how these results compare to actively practicing pediatricians in the community and the impact on access to care for CMC.
Figure 1
.png) Mean Perceived Relevance by PGY
Mean Perceived Relevance by PGYFigure 2
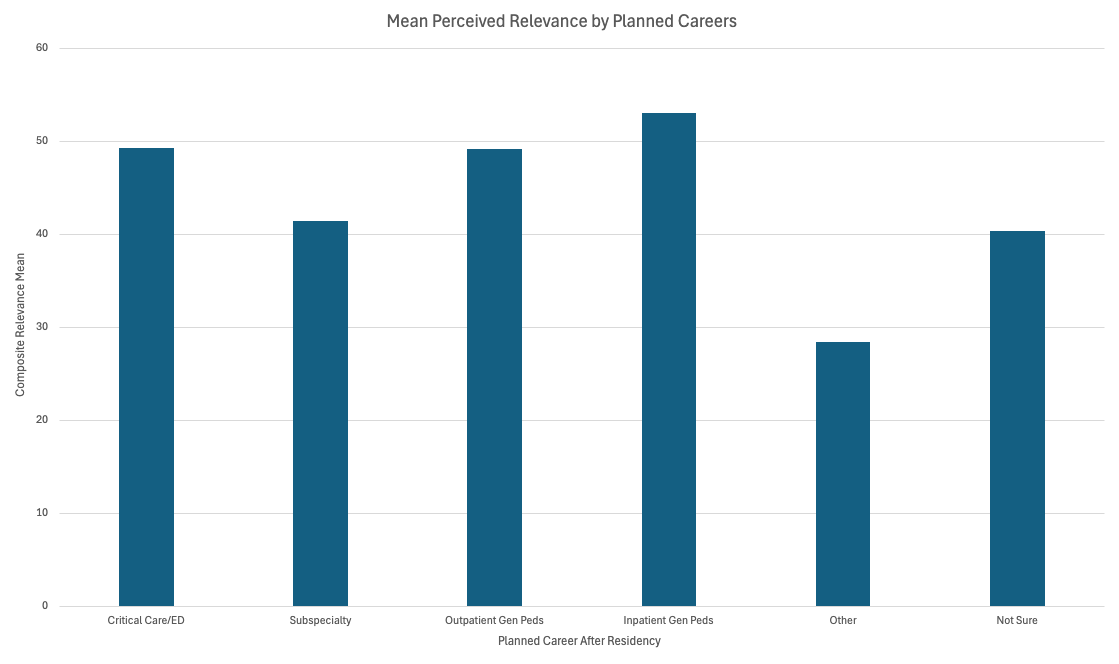 Mean Perceived Relevance by Planned Career
Mean Perceived Relevance by Planned CareerFigure 1
.png) Mean Perceived Relevance by PGY
Mean Perceived Relevance by PGYFigure 2
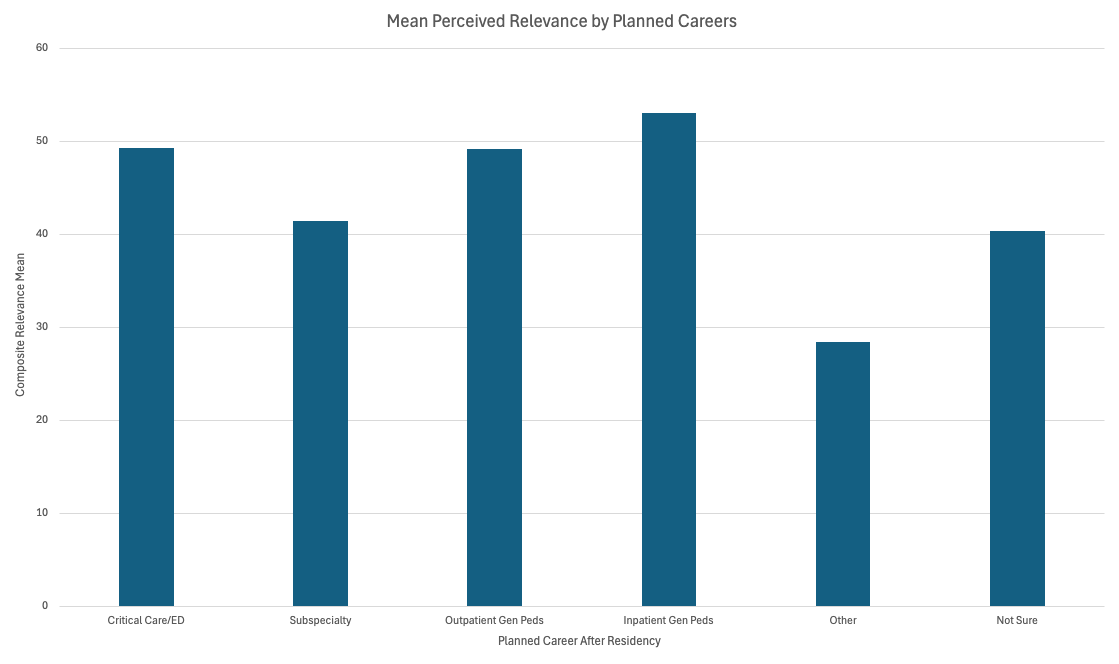 Mean Perceived Relevance by Planned Career
Mean Perceived Relevance by Planned Career
