Emergency Medicine 14
Session: Emergency Medicine 14
569 - Comparative Analysis of TWIST Scores in Pediatric Patients (<18 years) Presenting with Acute Testicular Pain: Testicular Torsion vs. Appendix Testis Torsion
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 569.4058
Maryam M. Hockley, Phoenix Children's Hospital, Phoenix, AZ, United States; Daniel Salevitz, Mayo Clinic Alix School of Medicine, Phoenix, AZ, United States; Nicolette G. Payne, Phoenix Children's Hospital, Phoenix, AZ, United States; Samuel H. Dowell, Phoenix Children's Hospital, Phoenix, AZ, United States; Stephanie Miller, Creighton University School of Medicine, Phoenix, AZ, United States; Cecilia Monteilh, Phoenix Children's Hospital, Phoenix, AZ, United States; Gwen Marie. Grimsby, Phoenix Children's Hospital, Phoenix, AZ, United States

Maryam M. Hockley, MD, MPH (she/her/hers)
PEM Fellow
Phoenix Children's Hospital
Phoenix, Arizona, United States
Presenting Author(s)
Background: Acute scrotal pain is a frequent concern in pediatric emergency departments (PEDs). While testicular torsion (TT) necessitates surgical intervention, other causes of acute scrotal pain like appendix testis torsion (ATT) are managed conservatively. Distinguishing between these conditions based on signs and symptoms is challenging due to their overlap. The Testicular Workup for Ischemia and Suspected Torsion (TWIST) score may aid in the rapid identification of TT and potentially bypass the need for ultrasound which could shorten time to surgery and increase testicular salvage. The goal of this study was to compare TWIST scores in patients with TT versus ATT.
Objective: This study aims to determine whether a TWIST score of ≥5 is specific for TT compared to ATT in pediatric patients. Additionally, it evaluates the sensitivity and specificity of the TWIST scoring system across low, intermediate, and high-risk categories.
Design/Methods: A retrospective review was performed of patients < 18 years presenting with acute scrotal pain due to TT or ATT at a single, tertiary PED from 2007 to 2024. Patients were excluded if they lacked a documented exam, had other diagnoses, or presented directly to urology clinic. Age and each component of the TWIST was compared with t-tests.
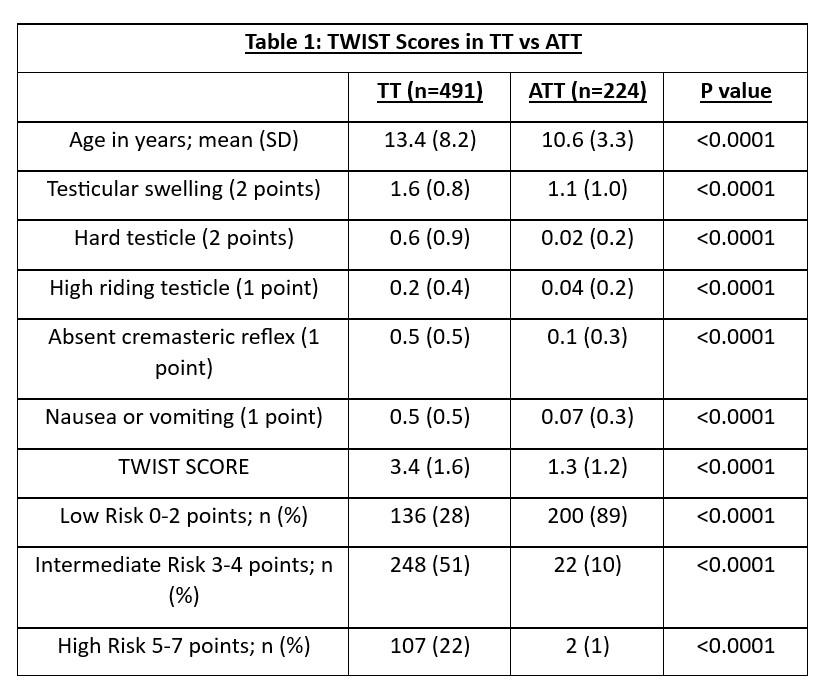
Results: 715 patients were included with a mean age of 12 (SD 7), 46% Caucasian, 57% Hispanic. 491 (69%) had TT and 224 (31%) ATT. Patients with TT were significantly older and had a significantly higher TWIST score than those with ATT (Table 1). High-risk scores (≥5) were associated with TT in 98% of cases. Intermediate to high-risk scores correlated with a sensitivity of 72%, while low-risk scores had a specificity of 89% for ruling out TT.
Conclusion(s): Pediatric patients with high TWIST scores are significantly more likely to have TT compared with ATT. 98% of patients with a TWIST greater than 5 had a true TT. This suggests that TWIST scoring could be a useful tool for prioritizing patients for surgical intervention, potentially reducing the reliance on ultrasound and decreasing time to OR.
Table 1: TWIST Scores in TT vs. ATT
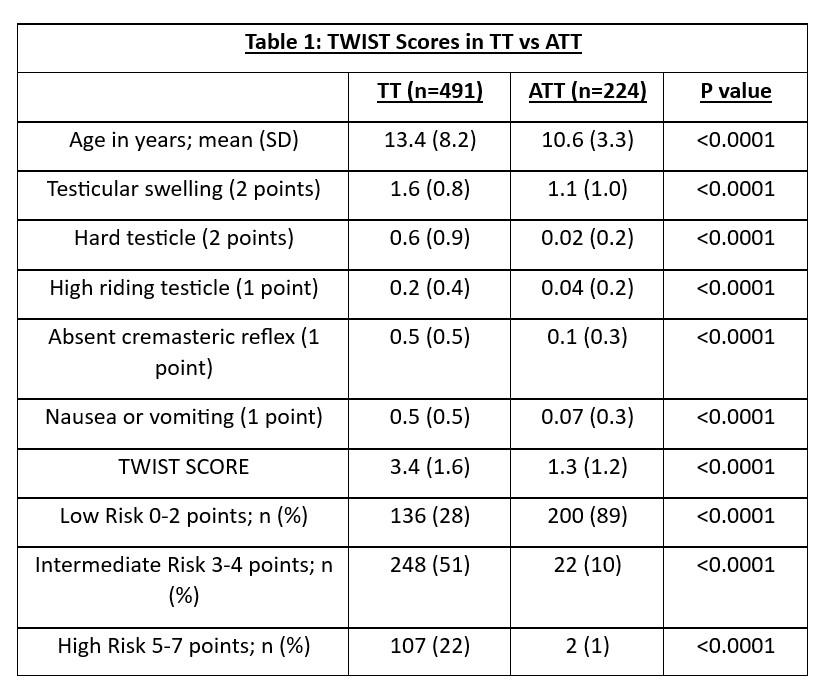
Table 1: TWIST Scores in TT vs. ATT