Emergency Medicine 11
Session: Emergency Medicine 11
524 - Current State Analysis – Identifying Quality Gaps Impacting Pediatric Neurotrauma Care
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 524.4066
Marie-Pier Lirette, The Hospital for Sick Children, coogee, New South Wales, Australia; Lynsey Downing, University of Toronto Temerty Faculty of Medicine, Toronto, ON, Canada; Sheila Rowed, The Hospital for Sick Children, Toronto, ON, Canada; Joshua K. Ramjist, The Hospital for Sick Children, Toronto, ON, Canada; Suzanne Beno, The Hospital for Sick Children, Toronto, ON, Canada
.jpg)
Marie-Pier Lirette, MBChB (Hons), MSc (she/her/hers)
Fellow
The Hospital for Sick Children
coogee, New South Wales, Australia
Presenting Author(s)
Background: Traumatic brain injury (TBI), a leading etiology of pediatric mortality/morbidity, requires effective timely neuroprotective care to improve outcomes. Enhancing neurotrauma management through reducing Emergency Department length of stay (ED LOS) and improving timeliness of CT imaging and operating room (OR) readiness, is crucial.
Objective: We aimed to identify quality gaps influencing ED LOS and time to intubation, CT imaging and definitive management in isolated severe pediatric TBI.
Design/Methods: Multi-source baseline analysis was conducted including retrospective chart review and prospective time series analysis of trauma video recordings (TVRs) for patients with severe TBI that presented to our pediatric trauma center between January 2021 and December 2022. Primary outcome was ED LOS and secondary outcomes included time to intubation, CT imaging and craniotomy. Data was compared to existing benchmarks from the American College of Surgeons (ACS) and Pediatric Trauma Quality Improvement Program (TQIP). Front-line provider surveys and semi-structured stakeholder interviews were performed to identify quality gaps. The Model for Improvement was followed, and QI tools were developed to understand current state and guide future initiatives
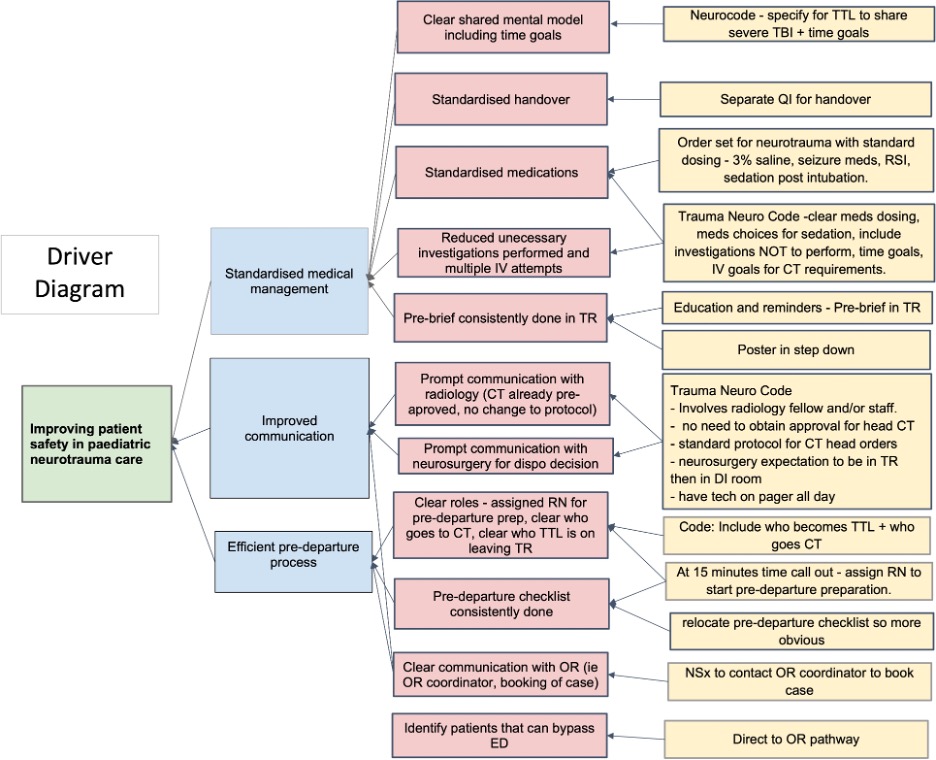
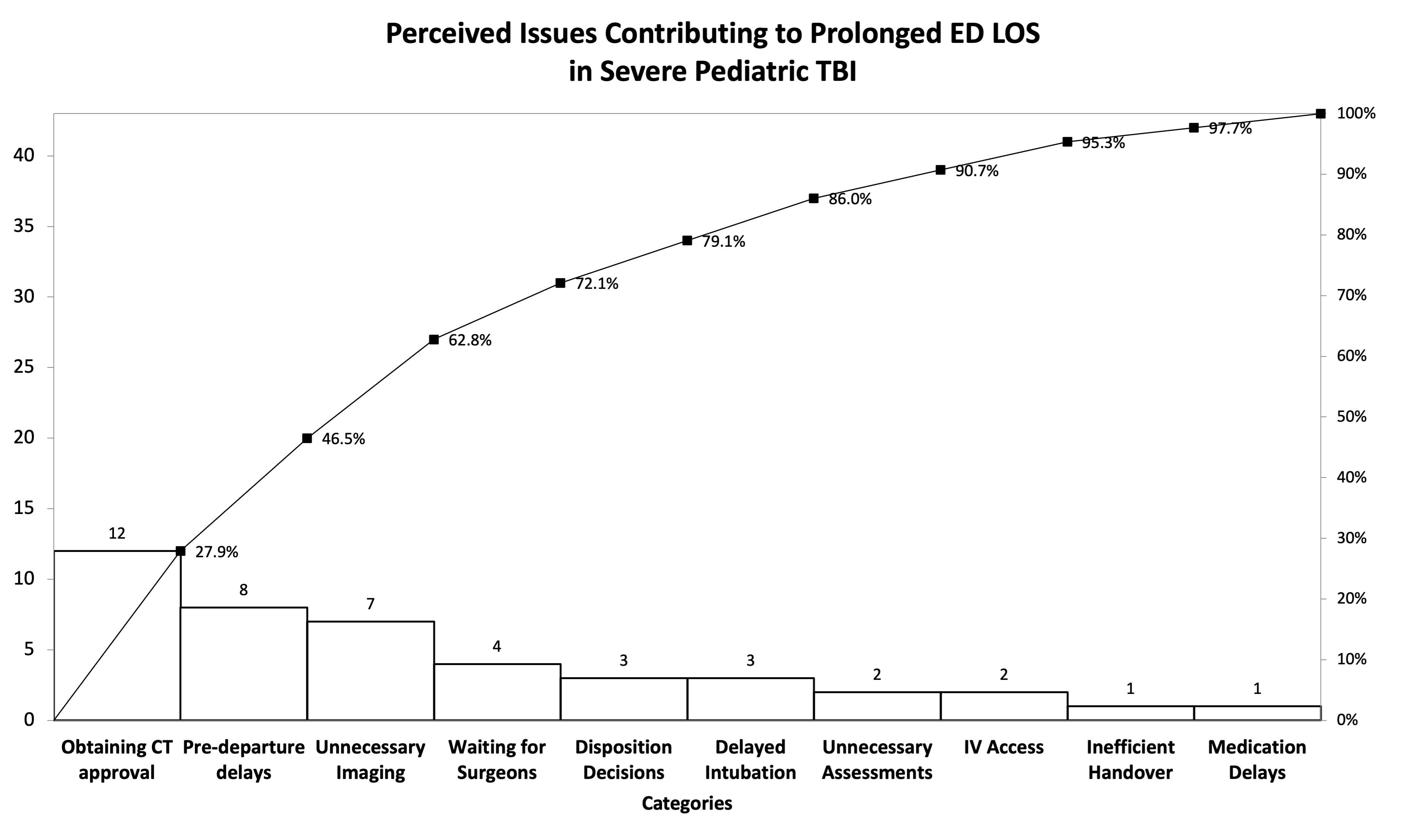
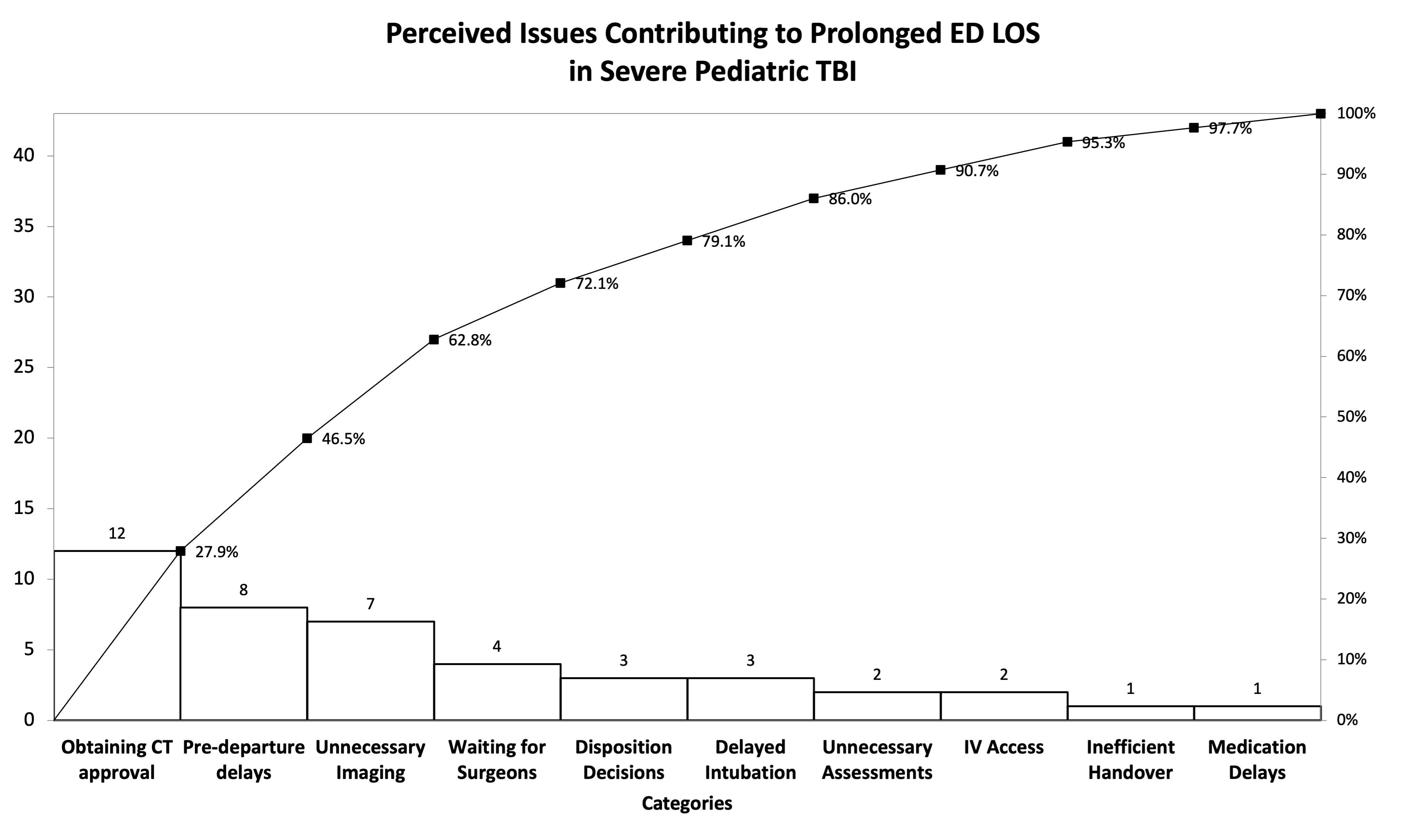
Results: Thirteen charts and five TVRs were retrospectively analyzed. Median ED LOS was 32 minutes, and times to intubation, CT and OR were 11.5, 44.5 and 103.5 minutes respectively (Table 1). 3/13 (23%) patients’ ED LOS met the institutional benchmark of < 20 minutes, 1/4 (25%) were intubated within 10 minutes and no patients had CT imaging initiated within 15 minutes from request. The majority of patients requiring craniotomy (4/6, 67%) occurred within the goal timeframe. Thirty-three providers completed the anonymous online survey and 14 stakeholders were interviewed. Thematic analysis revealed five key improvement areas: clinical management, communication, ED departure processes, and CT/OR readiness. A pareto chart identified specific quality gaps to target (Figure 1). The data gathered was instrumental in developing a driver diagram to guide further QI work (Figure 2), including development of a novel neurotrauma code.
Conclusion(s): This multi-source baseline analysis identified important quality gaps contributing to delayed care in severe isolated TBI. This study highlights the importance of a robust current state analysis to guide future QI work and ultimately improve pediatric neurotrauma care through meeting time-based international benchmarks.
Table 1 - Baseline Data for Severe TBI at The Hospital for Sick Children between 2021-2022
.jpg)
Figure 1 - Pareto Chart: Perceived Issues Contributing to Prolonged ED LOS in Severe Pediatric TBI
Driver Diagram: Improving Patient Safety in Severe Pediatric Neurotrauma Care
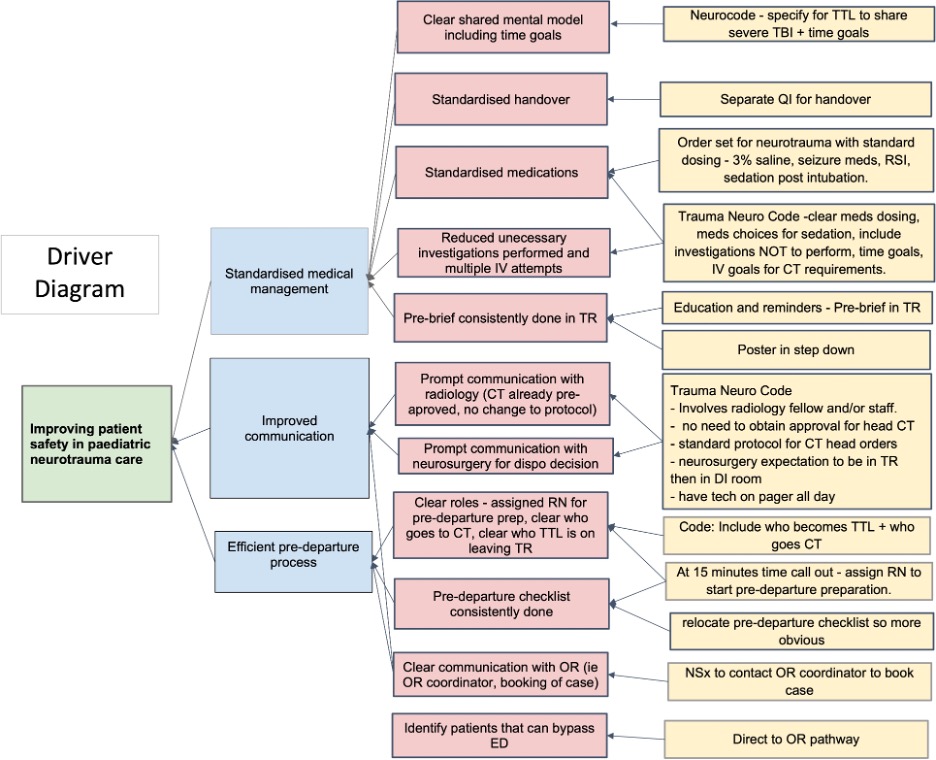
Table 1 - Baseline Data for Severe TBI at The Hospital for Sick Children between 2021-2022
.jpg)
Figure 1 - Pareto Chart: Perceived Issues Contributing to Prolonged ED LOS in Severe Pediatric TBI
Driver Diagram: Improving Patient Safety in Severe Pediatric Neurotrauma Care