Health Equity/Social Determinants of Health 11
Session: Health Equity/Social Determinants of Health 11
210 - An Analysis of Skin Color Representation in a Popular 2024 Pediatric Boards Resource
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 210.4026
Alyson Lee, University of Pittsburgh School of Medicine, Pittsburgh, PA, United States; Jonathan C. Li, UPMC Childrens Hospital of Pittsburgh, Pittsburgh, PA, United States; Talya F. Mandelkern, Boston Children's Hospital, Boston, MA, United States

Talya F. Mandelkern, MD (she/her/hers)
Attending Hospitalist
Boston Children's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Dermatology is a vital part of pediatric care - often serving as the first sign of systemic conditions such as autoimmune disorders, infection, malignancy, and child abuse/neglect. Studies have repeatedly demonstrated a paucity of medical education materials (MEMs) with diverse skin tones; most resources contain fewer than 25% of images with brown and black skin (1,2). This is disparate to our patient populations where nearly 40% identify as Black, LatinX, Asian, or Indigenous (3). Disparities in clinicians' ability to identify common diseases on skin of color compared to white skin leads to delays in diagnosis and worse outcomes for patients of color (4). Curricula with diverse images have been shown to improve clinical skills (5). Inequitable skin color representation in MEMs is therefore a form of systemic racism in medicine.
Objective: The American Academy of Pediatrics’ Pediatric Review and Education Program (PREP) is a leading educational resource for pediatricians preparing for boards and continuing education. This project aims to evaluate skin color representation in the PREP 2024 question bank.
Design/Methods: 267 questions were reviewed and all images showing skin were identified. Three raters independently scored skin tone using the NIS Skin Color Scale, a tool developed to assess skin color of research participants (1 to 10, 10 = darkest tone) (6). Scores were grouped: 1-2 light/white, 3-5 medium/brown, 6-10 dark/black (1). Images categorized differently between raters were grouped as light-medium or medium-dark. Interrater reliability in skin color grouping was assessed using Kappa with >0.75 excellent, 0.4-0.75 good, and < 0.4 marginal (7).
Results: N=61 clinical images were identified for review. Two were excluded due to insufficient skin to score. Skin color scores for all raters ranged from 1-7. N=42 images were grouped the same by all raters (figure 1). Of N=17 non-unanimously scored images, 13 were designated light-medium and 4 medium-dark. No images scored light-dark. Figure 2 displays final groupings with 69% of images light or light-medium and only three images categorized dark (5%). All raters showed good interrater reproducibility for light, medium, and dark categories (figure 3).
Conclusion(s): Our study found a notable lack of darker/black skin tones in the PREP 2024 question bank compared to light/white skin. This represents a perpetuation of disparities in skin tone representation in MEMs. Addressing such inequities is an essential component of combating systemic racism in medicine. MEMs should aim to display images with equal representation of light, medium, and dark skin tones.
Figure 1
.png) Individual Rater Groupings
Individual Rater GroupingsFigure 2
.png) Combined Rater Groupings
Combined Rater GroupingsFigure 3
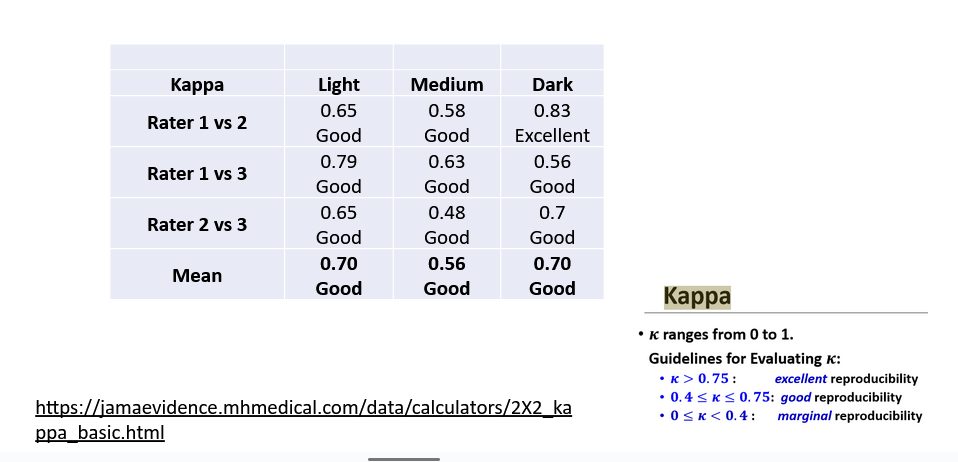 Interrater Reproducibility
Interrater Reproducibility
