Mental Health 3
Session: Mental Health 3
076 - Destigmatizing Mental Health Conversations among Chinese-American Parents and their Children through a Community-Based Parental Curriculum
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 76.4084
ALICE YU, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Larry Wang, Northwestern University The Feinberg School of Medicine, Chicago, IL, United States; Saaz Malhotra, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Isabelle Kang, Northwestern University Feinberg School of Medicine, Chicago, IL, United States; Catherine Chen, Northwestern University The Feinberg School of Medicine, Chicago, IL, United States; Mary Nielson, Northwestern University The Feinberg School of Medicine, Chicago, IL, United States; Emily L. Lam, Northwestern University The Feinberg School of Medicine, Chicago, IL, United States; Kristin Kan, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States

ALICE YU, MD (she/her/hers)
Resident Physician
Ann & Robert H. Lurie Children's Hospital of Chicago
Chicago, Illinois, United States
Presenting Author(s)
Background: Asian-American children are at-risk for developing mental health issues for a wide array of reasons, including ethnic and cultural socialization, familism, discrimination, and education-related stress. Literature shows that disempowering communication exacerbates mental health issues, including anxiety and depression. There is a need to destigmatize mental health conversations between Asian-American parents and children.
Objective: To develop a community-based, educational intervention with Chinatown parents to increase parents' comfort discussing mental health with children and ability to recognize signs of anxiety, depression, and suicidality.
Design/Methods: We piloted two 60-minute workshops with parents of Chicago Chinatown youth via a community parent mentoring program in May 2024. 1st workshop: guided group discussion after watching a personal narrative video of an Asian parent and child's journey to understanding mental health. 2nd workshop: presentation on pediatric depression, anxiety, and suicidality followed by role-play exercise simulating mental health discussions between adults and children. Workshops were conducted in Mandarin. Surveys were administered pre-, post-, and 2-months post-workshops. Likert-scale questions measured parents' comfort and likelihood to discuss mental health with children or adults and confidence to recognize anxiety, depression, and suicidality. Median scores of the Internalized Stigma of Mental Illness Inventory (ISMI-10) questionnaire were compared by Wilcoxon test. Summary statistics included median and interquartile ranges for questions on comfort, likelihood, and confidence. Proportions were reported for parental satisfaction with the workshops.
Results: Participants (n=33) were all women (100%) born outside the U.S (100%), and most married (96%) (Table 1). ISMI-10 scores significantly decreased between pre- and 2-month post-intervention (2.4 [2.2,2.6] v. 2.1 [2,2.3]; p< 0.01). No significant changes were observed in parents’ confidence, comfort, or likelihood of discussing mental health concerns with children (Table 2). Post-intervention feedback remained consistently positive by 2-month follow-up (Table 3).
Conclusion(s): This community-based pilot with Chinatown parents addressed a critical gap in building parents' comfort to engage in mental health conversations with their children. We found this intervention significantly reduced self-reported internal stigma among participants 2 months after workshops. Future steps include scaling the curriculum for wider implementation and understanding what parents further seek to destigmatize mental health conversations.
Table 1: Participant Demographics
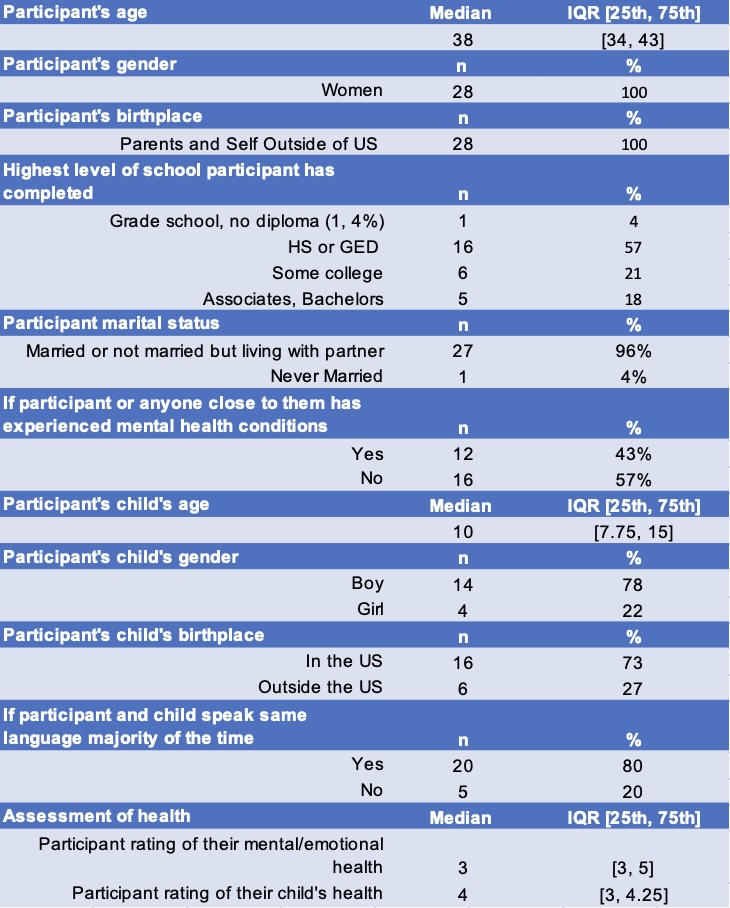
Table 2: Mental Health Discussion Comfort/Confidence/Likelihood Questionnaire
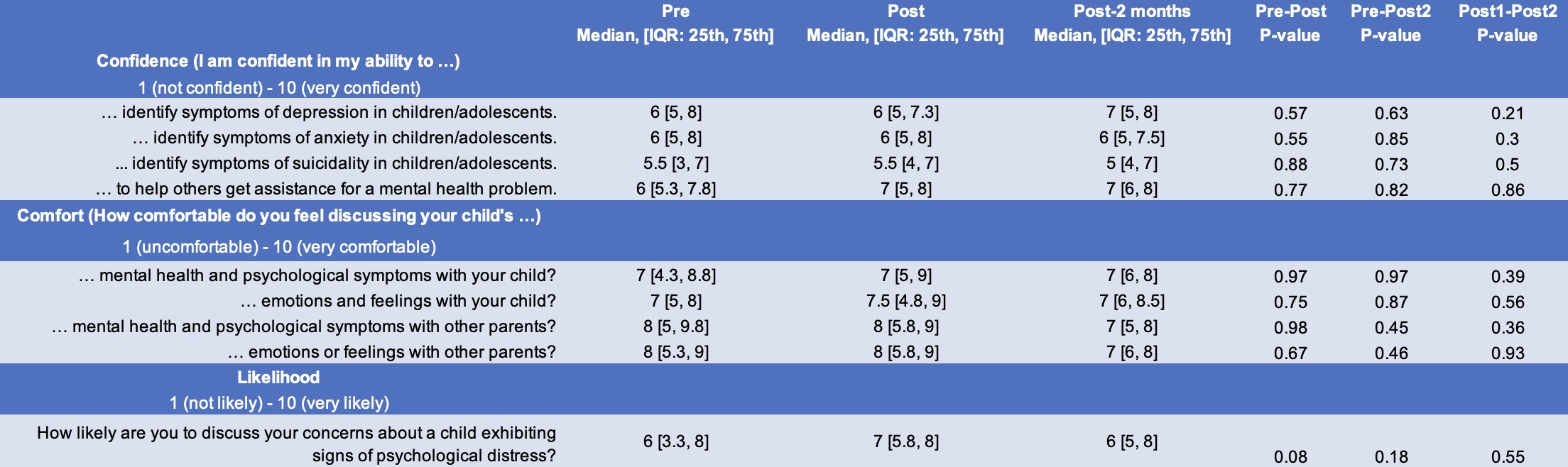
Table 3: Post-curriculum Feedback
.jpg)
Table 1: Participant Demographics
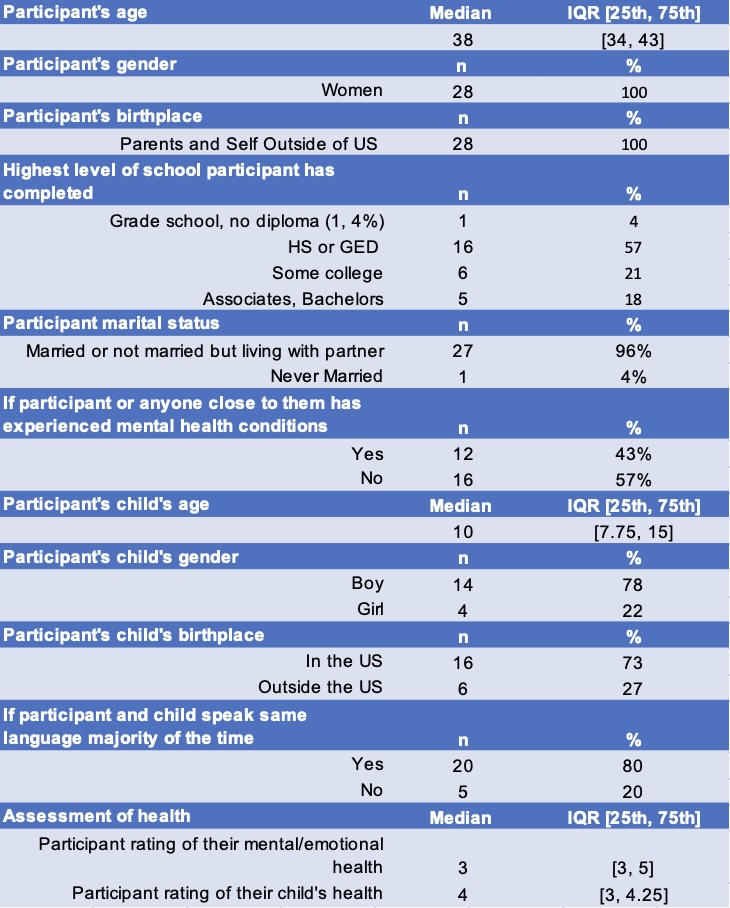
Table 2: Mental Health Discussion Comfort/Confidence/Likelihood Questionnaire
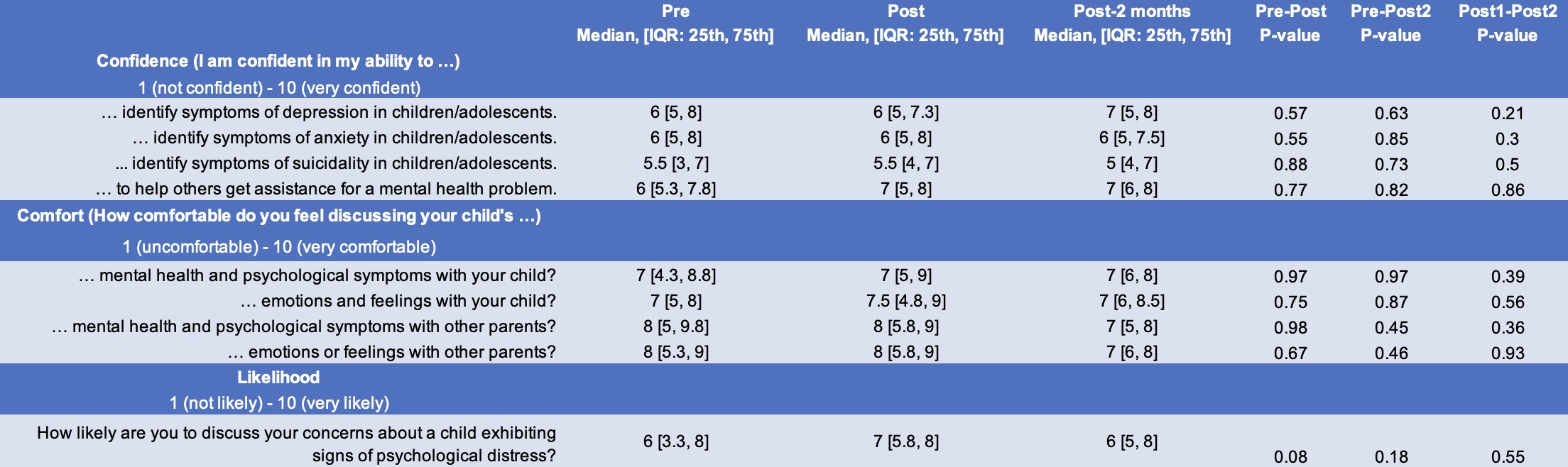
Table 3: Post-curriculum Feedback
.jpg)

