Health Equity/Social Determinants of Health 9
Session: Health Equity/Social Determinants of Health 9
179 - "He was not listening to hear me": Physician Communication and Parent Inclusion and Marginalization in the Pediatric Emergency Department
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 179.3572
Colleen K. Gutman, University of Florida College of Medicine, Gainesville, FL, United States; Antionette McFarlane, University of Virginia School of Medicine, Charlottesville, VA, United States; Rosemarie Fernandez, University of Florida College of Medicine, Gainesville, FL, United States; K. Casey Lion, University of Washington/ Seattle Children's Hospital, Seattle, WA, United States; Paul L. Aronson, Yale School of Medicine, New Haven, CT, United States; Carma Bylund, University of Florida College of Medicine, gainesville, FL, United States; Nancy Joseph, University of Florida College of Medicine, Gainesville, FL, United States; Carla L. Fisher, University of Florida College of Medicine, Gainesville, FL, United States

Colleen K. Gutman, MD (she/her/hers)
Assistant Professor
University of Florida College of Medicine
Gainesville, Florida, United States
Presenting Author(s)
Background: Inequities in pediatric emergency department (ED) care may be influenced by disparities in clinician communication.
Objective: We sought to examine, from the perspective of parents from marginalized racial and ethnic backgrounds, how clinician-parent communication is characterized during pediatric ED visits.
Design/Methods: We conducted and analyzed in-depth semi-structured individual interviews with parents and caregivers (“parents”) of pediatric ED patients from marginalized racial and ethnic backgrounds. We applied a constant comparative method approach to conduct a thematic analysis informed by grounded theory. To ensure rigor, we collected and analyzed data concurrently. We used the patient-centered communication (PCC) framework and the ten principles of Public Health Critical Race Praxis as sensitizing constructs during analysis. Two coders followed several analytical steps: 1) discovery of concepts (i.e., open coding), 2) identification of themes by grouping concepts, 3) axial coding to identify thematic properties, and 4) identification of exemplar excerpts for rich description. Thematic saturation was based on repetition, recurrence, and forcefulness.
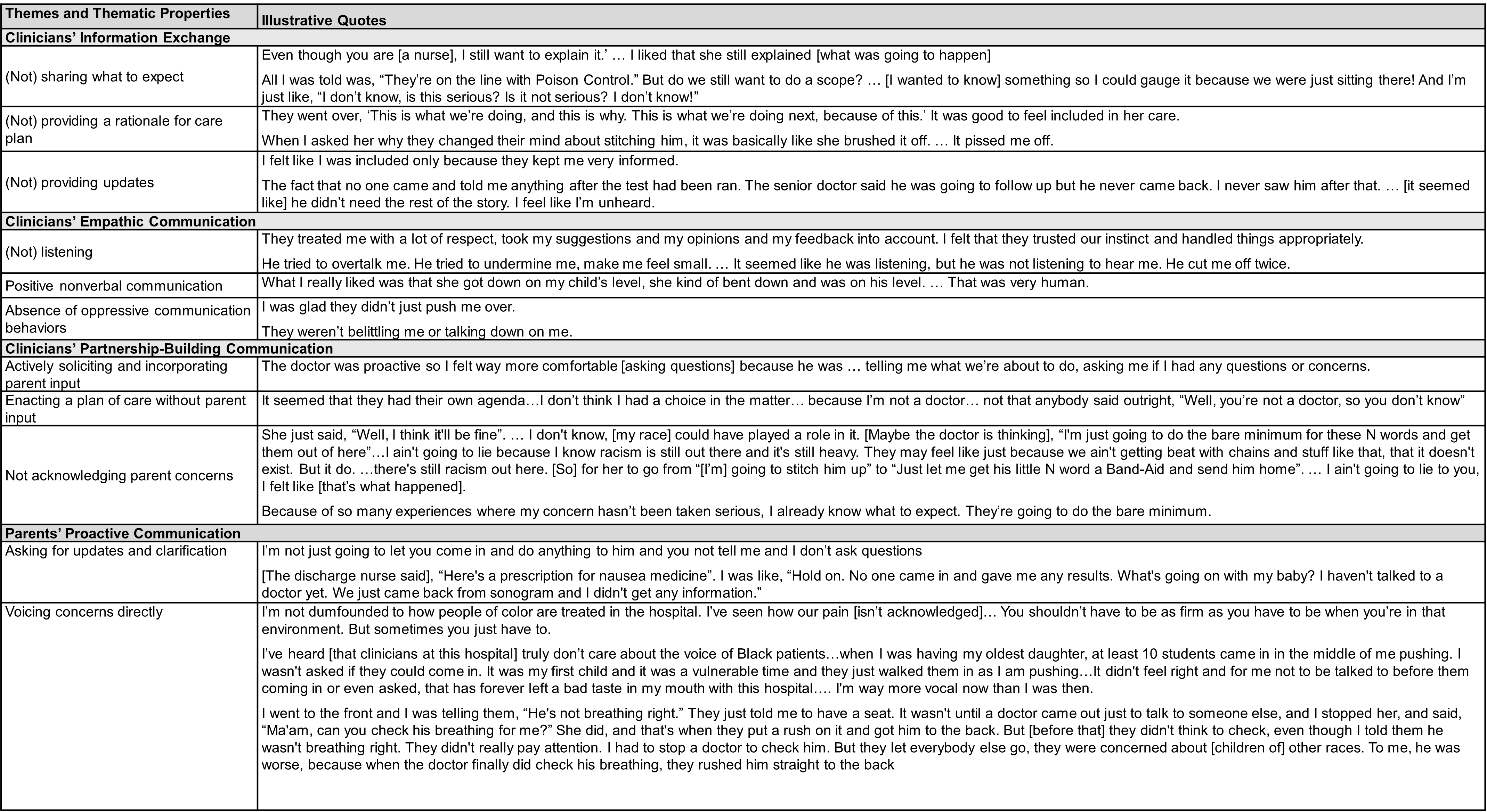
Results: Nineteen parents from a single academic pediatric ED participated (Table 1). Parents described three clinician communicative behaviors that facilitated their sense of inclusion or marginalization (Table 2): information exchange, empathic communication, and partnership-building. Parents also stressed the importance of their own proactive communication in facilitating their inclusion. Although few parents described experiencing racism during their child’s ED visit, many had during other healthcare encounters. Some parents explicitly drew from those experiences when describing how they received and responded to gaps in PCC. Yet even those parents who did not explicitly describe experiencing racism used language (such as feeling “brushed off” and “unheard”) that suggests a position of marginalization within unequal power dynamics in the interaction. In particular, parents described how their use of proactive communication was motivated by their past experiences of racism in medical encounters.
Conclusion(s): The presence or absence of PCC meaningfully impacts parents’ experiences communicating with pediatric ED clinicians. When viewed with a race conscious lens, these narratives demonstrate ways in which experienced racism, both past and present, may inform how parents receive and respond to gaps in PCC. PCC-focused interventions that adapt a race-conscious perspective may have a role in promoting health equity.
Table 1. Characteristics of Participants
.png)
Table 2. Themes, thematic properties, and illustrative quotes
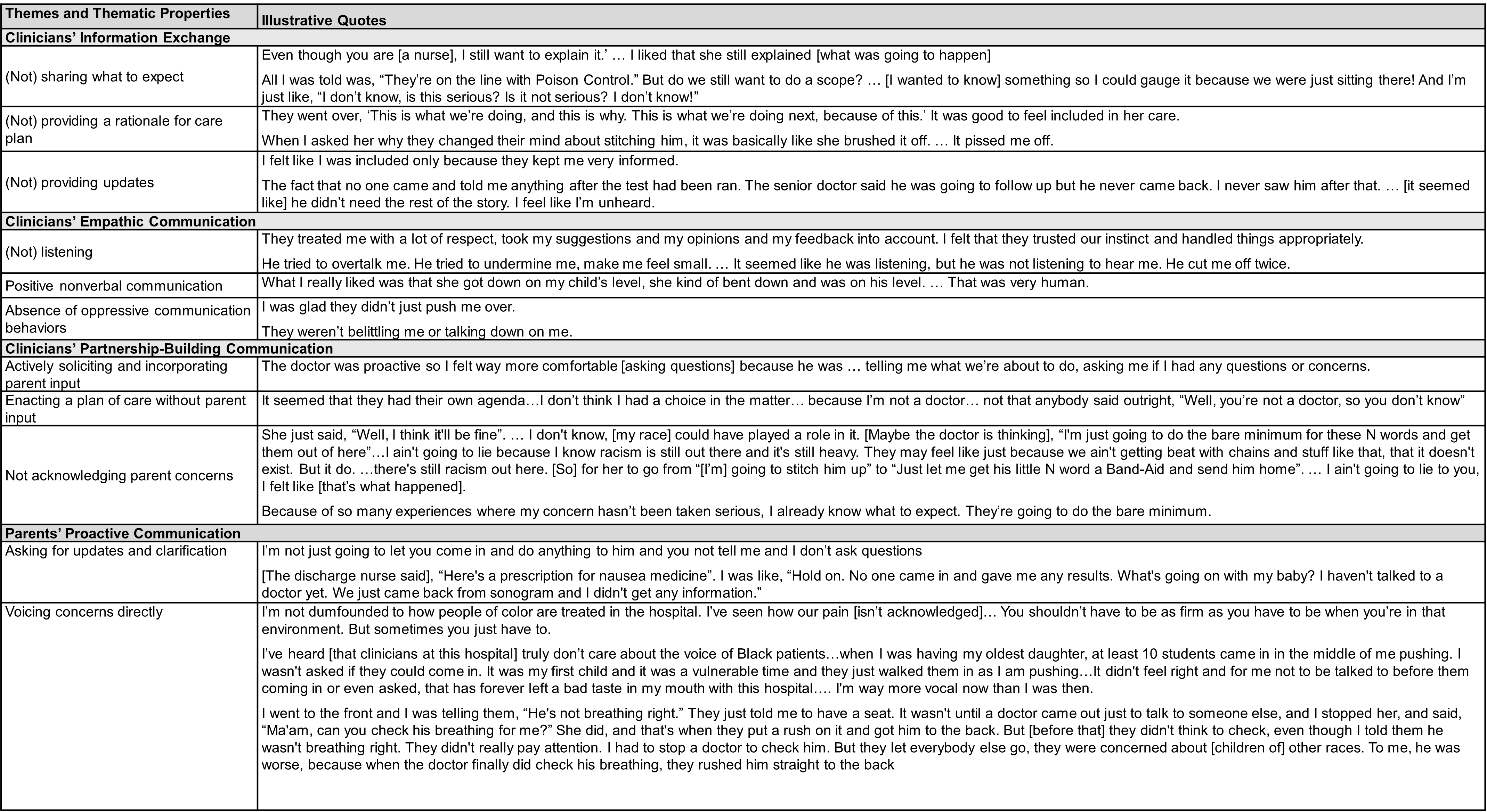
Table 1. Characteristics of Participants
.png)
Table 2. Themes, thematic properties, and illustrative quotes