Neonatal Pulmonology - Basic/Translational Science 3
Session: Neonatal Pulmonology - Basic/Translational Science 3
312 - Association of Early Airway Protein Level and Gene Variants of the TSP-1 with Development of BPD in ELBW Infants- An Observational Cohort Study
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 312.3579
Parvathy Krishnan, Floating Hospital for Children at Tufts Medical Center, MA, MA, United States; Lance A.. Parton, MD, NYMC, Valhalla, NY, United States

Parvathy Krishnan, MD
Neonatologist
Floating Hospital for Children at Tufts Medical Center
MA, Massachusetts, United States
Presenting Author(s)
Background: The normal sequence of lung development is disrupted with premature birth resulting in the histologic pattern of alveolar simplification, impaired vascular growth, and alterations in the extracellular matrix. Thrombospondin-1 (TSP- 1) is an extracellular glycoprotein that mediates the differentiation of specialized stem cells into alveolar epithelial lineage-specific cells. TSP-1 triggers anti-inflammatory cytokine IL-10 production in macrophages. Since bronchopulmonary dysplasia (BPD) involves inhibition of lung development, differential expression of the THBS-1 gene may impact lung development and have an important role in BPD.
Objective: To examine the effects of variants of the Thrombospondin-1 gene (THBS1) and early airway TSP-1 protein expression in Extremely Low Birth Weight (ELBW) infants with and without BPD.
Design/Methods: This was a prospective observational, cohort study including ELBW infants with and without BPD. DNA was isolated from buccal swabs and subjected to RT-PCR with specific TaqMan probes for THBS1 gene variants. Airway TSP-1 protein expression was measured in tracheal aspirates collected within the first ten days subjected to ELISA. Chi-square and Fisher’s exact test were used for categorical variables. Wilcoxon Rank Sum and t-test were used for continuous variables; z-test for allele frequencies, with p< 0.05 statistically significant. The study was approved by IRB at New York Medical College.
Results: ELBW infants with BPD had significantly lower gestational ages and birth weights compared to those without BPD [25 (24,26) and 27 (25,28) weeks; median (IQR); p= 0.008] and [712 (155) and 820 (153) grams; mean (SD); p= 0.002], respectively. (Table 1) While individual genotype distributions were not different between No BPD and BPD groups, there were significant differences in the haplotype distributions of THBS1 variants rs2664139/rs1478604 (p=0.006) and THBS1 variants rs1478605/rs1478604 (p=0.008) even after adjusting for birth weight, male sex, NEC, IVH, and PDA treatment (0.02 and 0.04). (Table 2) There were also significant differences in airway TSP-1 protein levels between moderate and severe BPD patients [(p=0.02) (no BPD - 527 (114-1755); moderate BPD 312 (262-641); and severe BPD 211 (117-352) ng/dl; median (IQR)]. (Figure 1)
Conclusion(s): The combination of THBS1 variants was significantly associated with BPD. Early airway TSP-1 expression was significantly different between the non-BPD, moderate BPD, and severe BPD groups, with the most affected infants having the lowest airway TSP-1 expression. This implicates TSP-1 as a regulator of alveolar differentiation and repair.
Table 1: Demographic and clinical characteristics of the study population
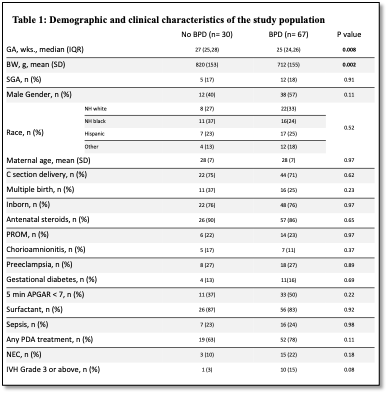 Table 1: Demographic and clinical characteristics of the study population
Table 1: Demographic and clinical characteristics of the study populationTable 2: Genotype distribution of the THBS1 gene variants in the study population
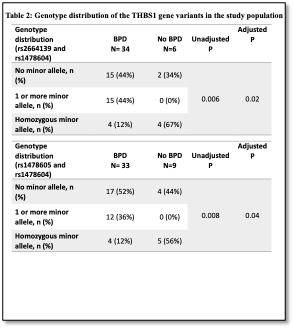 Table 2: Genotype distribution of the THBS1 gene variants in the study population
Table 2: Genotype distribution of the THBS1 gene variants in the study population Figure 1. Early airway TSP-1 protein expression in the study population
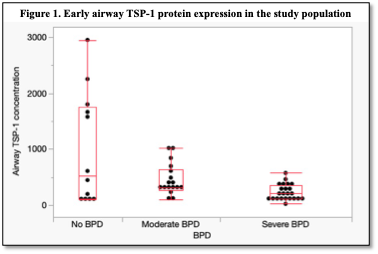 Figure 1. Early airway TSP-1 protein expression in the study population
Figure 1. Early airway TSP-1 protein expression in the study populationTable 1: Demographic and clinical characteristics of the study population
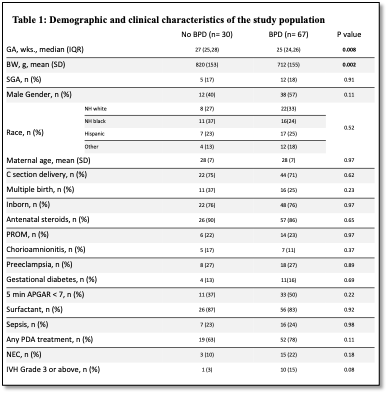 Table 1: Demographic and clinical characteristics of the study population
Table 1: Demographic and clinical characteristics of the study populationTable 2: Genotype distribution of the THBS1 gene variants in the study population
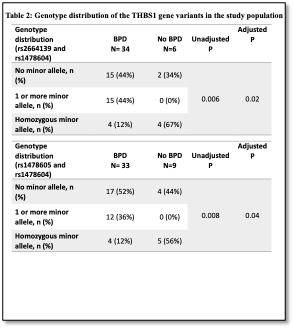 Table 2: Genotype distribution of the THBS1 gene variants in the study population
Table 2: Genotype distribution of the THBS1 gene variants in the study population Figure 1. Early airway TSP-1 protein expression in the study population
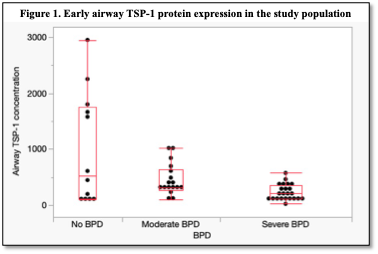 Figure 1. Early airway TSP-1 protein expression in the study population
Figure 1. Early airway TSP-1 protein expression in the study population
