Adolescent Medicine 3: E-Cigarettes & Other Substances
Session: Adolescent Medicine 3: E-Cigarettes & Other Substances
118 - Substance Use Services at Child Psychiatry Access Programs
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 118.6781
Alexis Ball, Seattle Children's, North Bend, WA, United States; Paige Tripp, University of California, San Francisco, School of Medicine, San Francisco, CA, United States; Chuan Mei Lee, University of California, San Francisco, School of Medicine, San Francisco, CA, United States; Jayme Congdon, University of California, San Francisco, School of Medicine, San Francisco, CA, United States
- AB
Alexis Ball, MD MPP
Acting Assistant Professor
Seattle Children's
North Bend, Washington, United States
Presenting Author(s)
Background: Adolescents are experiencing rapidly rising morbidity and mortality from substance use and yet have the least access to substance use related care. Child psychiatry access programs (CPAPs)—defined as centralized programs offering rapid remote pediatric mental health consultation for primary care physicians (PCPs)— are a coordinated care approach to address mental health workforce and access challenges by enhancing PCP's capacity to manage mental health conditions in primary care. Given the early success and growth of the statewide CPAP model, the inclusion of substance use within the scope of CPAP consultation services could rapidly expand urgently needed prevention and treatment for a large proportion of U.S. adolescents. However, the current capacity and availability of CPAPs for substance use related care is not known.
Objective: To examine the clinical support and resources offered for substance use related care within CPAPs
Design/Methods: We examined the proportion of U.S. and Canadian CPAPs (n=56) that offer clinical support and resources for substance use (i.e., screening and prevention, treatment, harm reduction). Data were drawn from publicly available program-level survey data from the National Network of Child Psychiatry Access Programs (NNCPAP) and from CPAP websites. To contextualize these data, we compare with the proportion of CPAPs that provide similar services and resources for depression, the most common pediatric behavioral health concern.
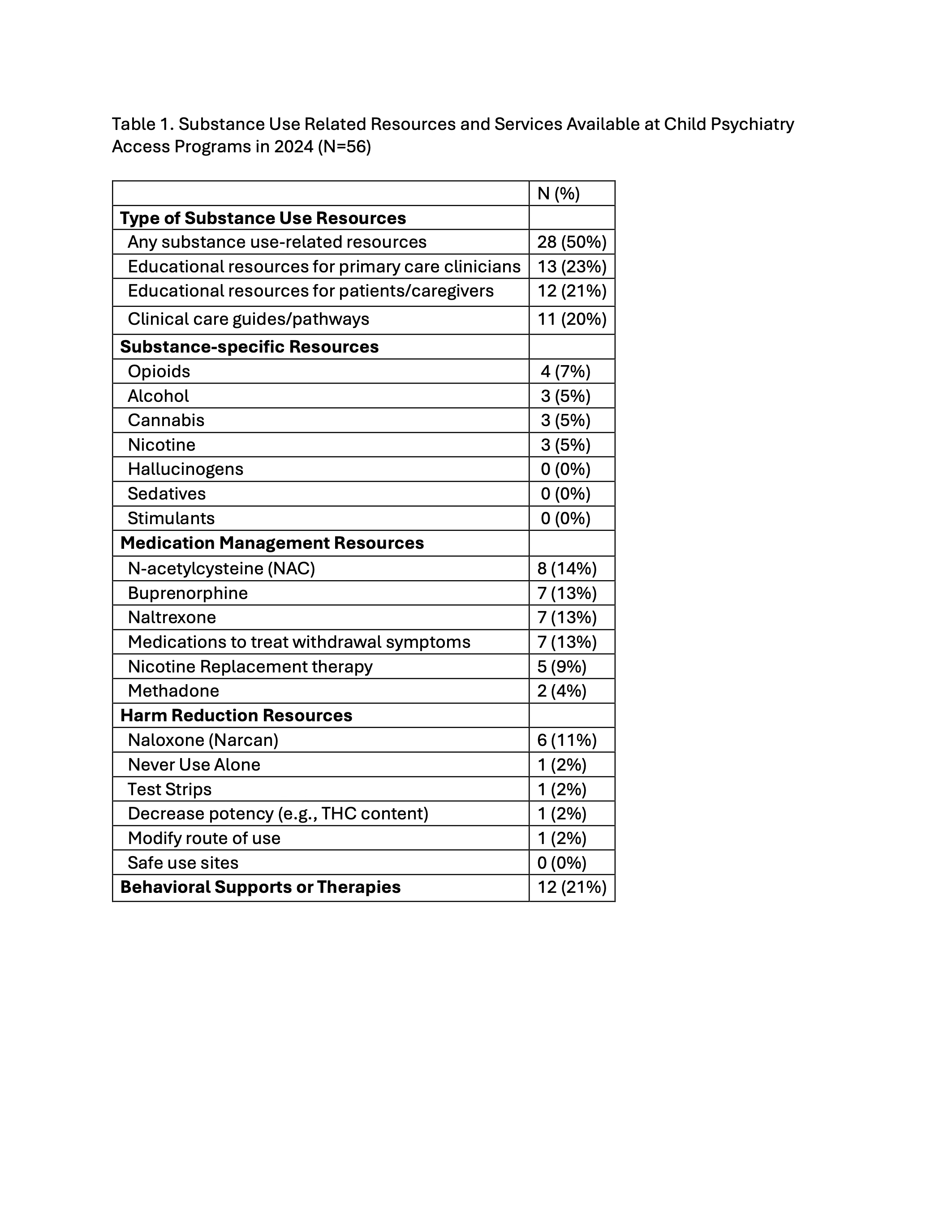
Results: Of 56 CPAPs, 28 (50%) offered any resources for substance use related care (Figure 1), 11 (20%) included a clinical pathway or direct link to another program’s pathway, and 8 (14%) provided guidance on some type of medication treatment (Table 1). Of the 11 CPAPs with clinical pathways for SUD treatment, 6 referenced harm reduction or overdose prevention strategies, with only one site offering strategies beyond naloxone. For comparison, 16 (29%) CPAPs provide clinical pathways for identifying and treating depression and 18 (32%) include specific antidepressant medication and dosing guidance.
Conclusion(s): Our findings showed that about half of CPAPs offer some type of resource to support primary care clinicians with substance use related care, yet far fewer CPAPs offer specific clinical guidance on evidence-based medication treatment or harm reduction strategies. These findings suggest that CPAPs remain a largely untapped model for expanding access to substance use related expertise and guidance.
Availability of Substance Use Related Care Resources at Child Psychiatry Access Programs* in 2024
.jpg) CPAP = Child Psychiatry Access Program; *British Columbia, not pictured above, has a CPAP with substance use resources and a clinical guide/pathways
CPAP = Child Psychiatry Access Program; *British Columbia, not pictured above, has a CPAP with substance use resources and a clinical guide/pathwaysSubstance Use Related Resources and Services Available at Child Psychiatry Access Programs in 2024