Emergency Medicine 11
Session: Emergency Medicine 11
525 - Decreasing the time to antibiotics for patients with sickle cell disease and fever in an emergency department
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 525.4270
Sarika K. Sheth, Rady Children's Hospital San Diego, San Diego, CA, United States; Daniel Roderick, Rady Children's Hospital San Diego, San Diego, CA, United States; Jenny M. Kim, Rady Children's Hospital San Diego, San Diego, CA, United States; Yvette Wang, Rady Children's Hospital San Diego, San Diego, CA, United States; Amy Bryl, Rady Children's Hospital/University of California San Diego, San Diego, CA, United States; Karen Yaphockun, Rady Children's Hospital San Diego/UCSD, San Diego, CA, United States

Sarika K. Sheth, MD (she/her/hers)
Assistant Clinical Professor
Rady Children's Hospital San Diego
San Diego, California, United States
Presenting Author(s)
Background: Patients with sickle cell disease are immunocompromised given their functional asplenia, leaving them at higher risk for bacteremia, particularly from encapsulated organisms. In 2011, an expert panel identified 41 quality indicators for the care of sickle cell disease patients, one of which was that sickle cell disease patients who have a fever of >38.5°C should be given parenteral broad spectrum antibiotic treatment within 60 min of triage.
Objective: Our aim was to decrease the time from arrival to antibiotics for patients with sickle cell disease with fever from 152 min to 60 minutes in 12 months.
Design/Methods: A quality improvement (QI) task force including emergency medicine and physicians and nurses, hematology physicians, informatics, and quality management was created. A baseline process was mapped to assess points at which antibiotics could be ordered and given to patients with sickle cell disease and fever. Electronic health record (EHR) interventions included modification of an existing order set and pathway, in addition to a best practice advisory alert. Educational interventions included nursing education and physician education through division presentations (Figure 1). Process measures include time from room to antibiotics as well as time from triage vital signs to antibiotics. We used statistical process control to analyze changes in measures over time.
Results: Time from arrival to antibiotics decreased from 152 minutes to 68 minutes within 5 months of project initiation (Figure 2). Time from patient being roomed to antibiotics decreased from 124 minutes to 55 minutes (Figure 3). Time from triage vital signs to antibiotics decreased from 140 minutes to 63 minutes within 5 months of project initiation.
Conclusion(s): Using QI methodology, we successfully decreased the time to antibiotics for patients with sickle disease presenting to the emergency department with fever.
Figure 1.
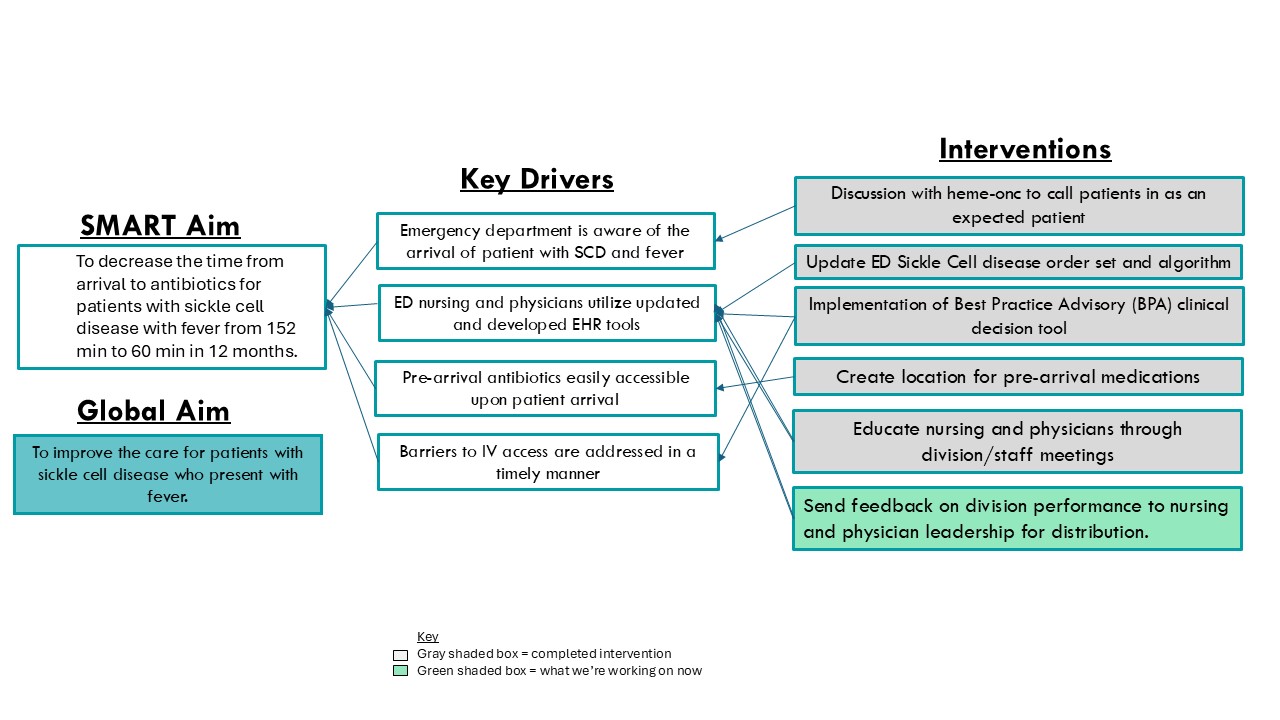 Key Driver Diagram
Key Driver DiagramFigure 2.
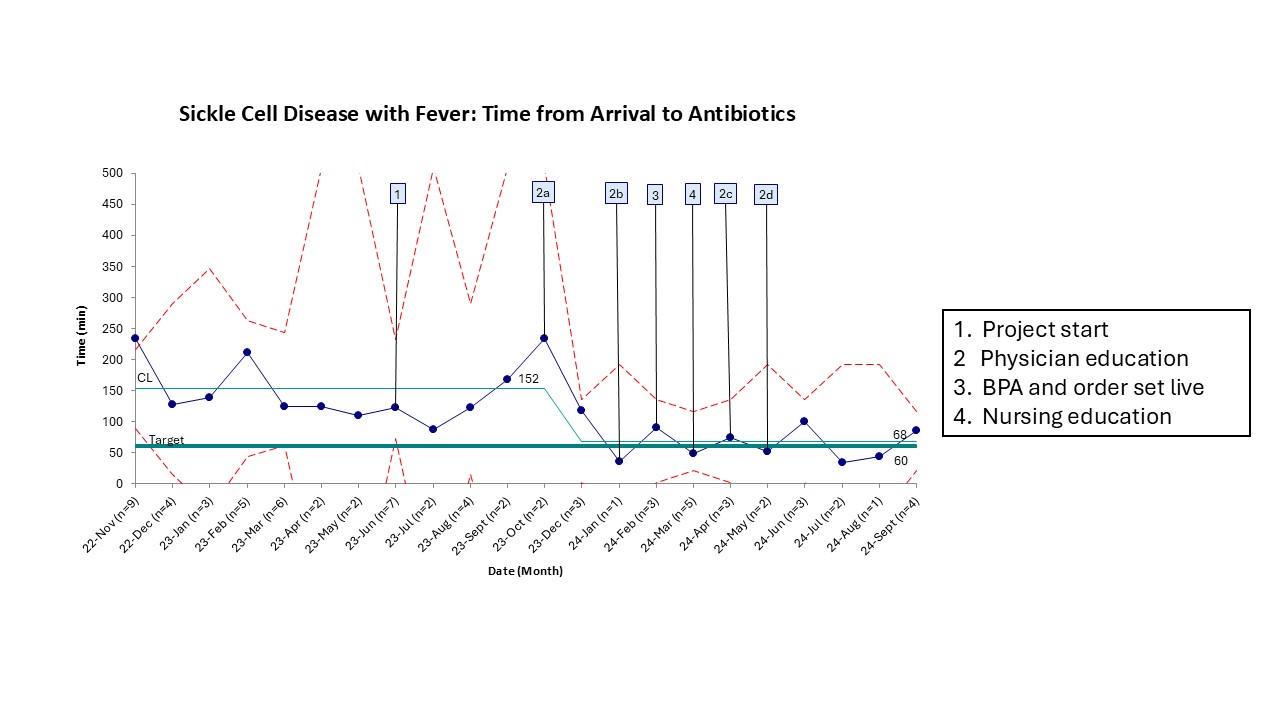 Sickle Cell Disease with Fever: Time from Arrival to Antibiotics
Sickle Cell Disease with Fever: Time from Arrival to AntibioticsFigure 3.
.jpg) Sickle Cell Disease with Fever: Time from Room to Antibiotics
Sickle Cell Disease with Fever: Time from Room to Antibiotics

