Children with Chronic Conditions 3
Session: Children with Chronic Conditions 3
463 - Surgical decision making in video-recorded clinical encounters for children with neuromuscular scoliosis: a qualitative study
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 463.6707
Jody L. Lin, University of Utah, Salt Lake City, UT, United States; Angela S. Zhu, University of Utah School of Medicine, Salt Lake City, UT, United States; Marla Clayman, Veterans Health Administration, Evanston, IL, United States; Kimberly Kaphingst, University of Utah, Salt Lake City, UT, United States; Kaleb Eppich, University of Utah School of Medicine, Salt Lake City, UT, United States; Gregory J. Stoddard, University of Utah, Salt Lake Cty, UT, United States; Lindsay Andras, Children's Hospital Los Angeles, Los Angeles, CA, United States; Unni Narayanan, The Hospital for Sick Children, Toronto, ON, Canada; Heather Keenan, University of Utah School of Medicine, Salt Lake City, UT, United States; Tamara D. Simon, Children's Hospital Los Angeles, Los Angeles, CA, United States; Steven Asch, Stanford University School of Medicine, Los Altos, CA, United States; Angie Fagerlin, University of Utah, Salt Lake City, UT, United States

Angela S. Zhu, ACRP-CP (she/her/hers)
Clinical Research Coordinator
University of Utah School of Medicine
Salt Lake City, Utah, United States
Presenting Author(s)
Background: Surgical treatment for neuromuscular scoliosis (NMS) is a decision with equipoise and thus ripe for shared decision making (SDM). What occurs during decision-making encounters is largely unknown.
Objective: This study aims to describe communication during surgical clinic visits for children with NMS and their relationship to SDM.
Design/Methods: We recruited English-speaking children aged 8-21 years with NMS, their adult caregivers, and their providers at an orthopaedic surgery consultation for NMS and video-recorded the visits. Two independent coders inductively analyzed each video using grounded theory through open coding, serial coding reviews, code and excerpt analysis to synthesize themes, and larger team meetings to finalize themes. Subsequently themes were deductively sorted within SDM domains of the DEEP-SDM qualitative coding scheme.
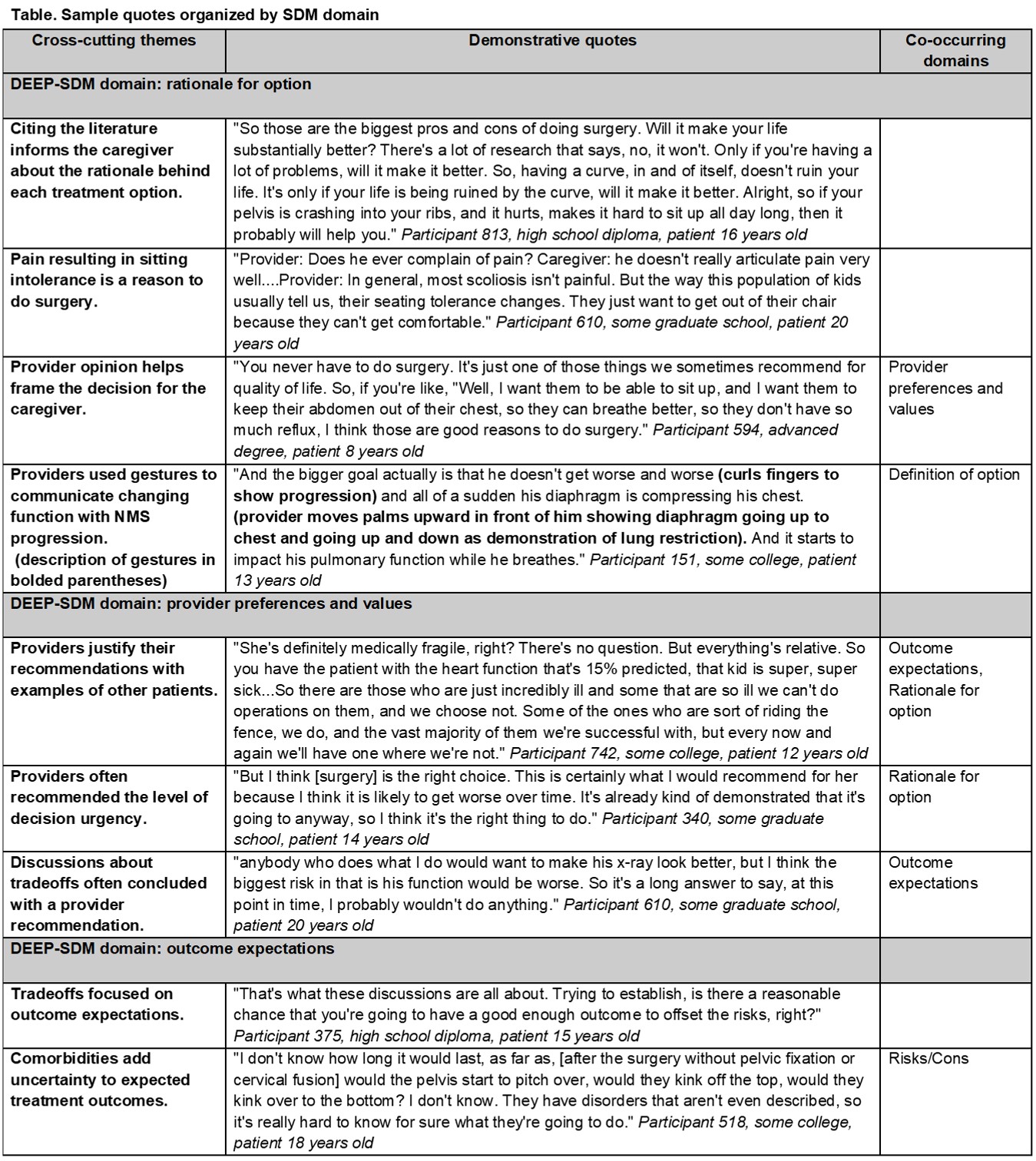
Results: In n=18 patient-caregiver-provider triads, patients had a mean age of 14.8 years [standard deviation (SD) 3.6 years] with 15 (83%) identifying as non-Hispanic White, 10 (56%) with technology dependence, and 12 (67%) with neurodevelopmental impairment. Caregivers had a mean age of 42.1 years (SD 5.2), with 17 (94%) identifying as White, and 15 (83%) with at least some college education. The n=3 providers comprised all surgeons who provide spinal fusion to treat NMS, were all male, and had 10-34 years of practice since residency. We synthesized nine themes (see Table for themes and quotes). While most themes cut across multiple SDM domains, we organized them under the most prominent domain. Notable themes include: 1) Providers often recommended the degree of decision urgency, particularly whether by deferring surgery the family would miss a window of opportunity for surgery. 2) Discussions about tradeoffs often concluded with a provider recommendation. Commonly discussed tradeoffs included improving sitting tolerance versus preserving mobility, surgical timing to optimize growth versus extent of surgical correction, and generally, balancing improved quality of life against risk for a bad outcome such as death. 3) Comorbidities add uncertainty to expected treatment outcomes. Interestingly, discussions about comorbidity-related uncertainty did not focus on how comorbidities affect the patient’s symptoms and thus the rationale for a particular treatment option. No themes fit the SDM domains of assessed patient/caregiver understanding or self-efficacy.
Conclusion(s): Surgical consults in our study focused on treatment rationale and provider preferences and less so on assessing caregiver understanding and self-efficacy.
Sample quotes organized by SDM domain