Emergency Medicine 13
Session: Emergency Medicine 13
563 - Think Outside The Bones: Non-Pharmacologic Interventions Can Improve Pain Scores in Patients with Forearm Fractures
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 563.6570
Jennifer Hockenbury, University of Louisville School of Medicine, Louisville, KY, United States; Alexander R. McMahan, Norton Children’s Hospital, Mount Washington, KY, United States; Kahir S. Jawad, Norton Children’s Hospital, Louisville, KY, United States; Theresa L. Kluthe, Norton Children's Medical Group - Louisville, KY, Louisville, KY, United States; Sandra Herr, Penn State Hershey, Jonestown, PA, United States; Adam Isacoff, University of Louisville School of Medicine, Louisville, KY, United States

Jennifer Hockenbury, MD (she/her/hers)
Pediatric Emergency Medicine Fellow
University of Louisville School of Medicine
Louisville, Kentucky, United States
Presenting Author(s)
Background: Pain and anxiety are common problems in the Pediatric Emergency Department (PED), often compounded by the chaotic environment, need for painful procedures, and stress of acute illness or injury. Failure to adequately address pain intensifies anxiety for the patient and their family, making PED evaluation and interventions more challenging. Pain is an inherently subjective multifactorial experience and should be assessed and treated as such. Non-pharmacologic pain management (NPPM) can supplement standard of care management by improving pain and procedural success, reducing stress and anxiety, and positively affecting patient and family satisfaction with their experience. However, NPPM remains underutilized in the PED.
Objective: Our goal was to incorporate NPPM into our PED and to specifically study whether these techniques could reduce pain scores in pediatric patients who sustained forearm fractures requiring sedated reduction. We hypothesized that in patients presenting to the PED with forearm fractures requiring sedated reduction, we would significantly reduce pain scores (assessed using Face, Legs, Activity, Cry, Consolability (FLACC) scale) by introducing the use of NPPM techniques during 2024 compared to standard of care management during 2023.
Design/Methods: We studied patients presenting to the PED with forearm fracture requiring sedated reduction during three months in 2023 compared to the same months in 2024. The intervention included integration of NPPM in the PED in 2024. Study design is pictorially shown using a Key Driver Diagram (Figure 1) and supplemented with a formal algorithm for incorporating NPPM into patient care (Figure 2). The primary outcome studied was difference in pain score: first score documented for a patient during their PED encounter compared with the patient’s score immediately prior to sedated reduction. Data were collected through retrospective chart review.
Results: The study included 228 patients, 110 pre-intervention and 118 post-intervention. Univariate comparisons of these patients found no significant differences between groups. When controlling for age, time to sedation, administration of analgesia, and time to analgesia, post-intervention patients had significantly higher odds of an improvement in their pain scores, OR = 2.381 (1.282, 4.522) p-value = 0.007 (Table 1).
Conclusion(s): Findings from this study encourage the use of NPPM to supplement standard of care management for patients who have sustained forearm fractures in the PED.
Figure 1
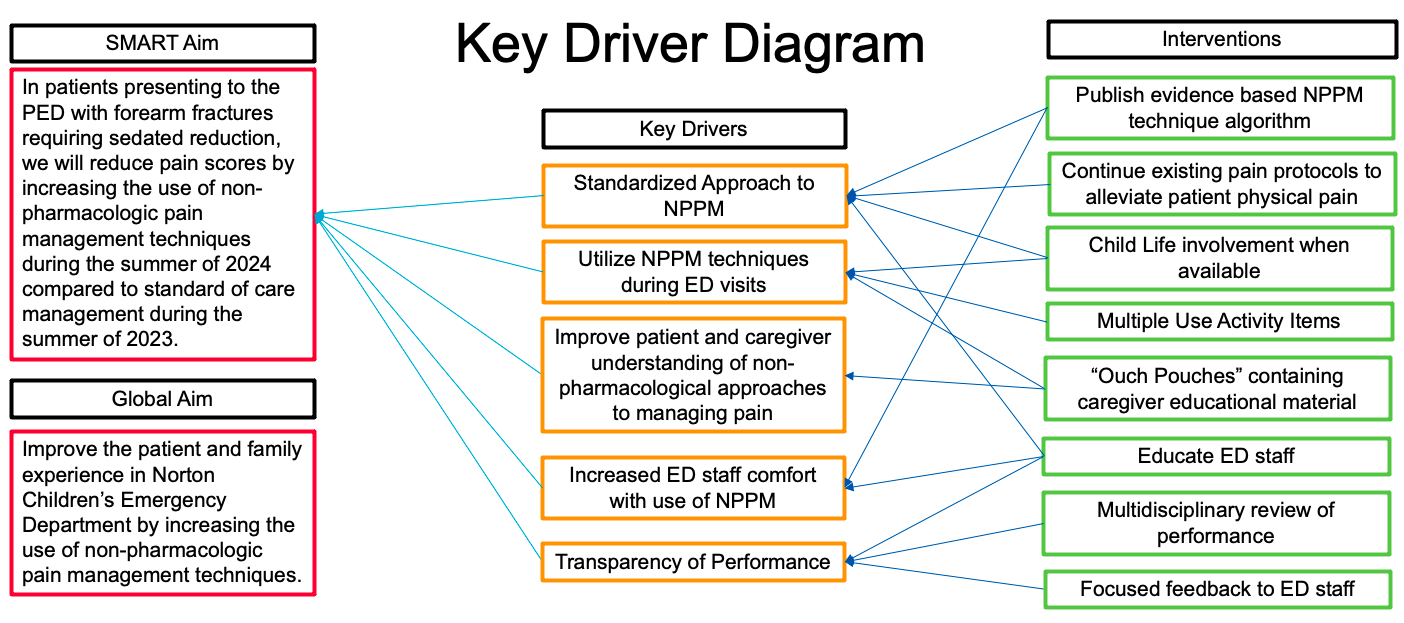 Study Design Key Driver Diagram.
Study Design Key Driver Diagram.Figure 2
.png) Non-Pharmacologic Pain Management Algorithm.
Non-Pharmacologic Pain Management Algorithm.Table 1
.jpg) Multivariate binomial regression predicting if a subject found improvement in their FLACC score.
Multivariate binomial regression predicting if a subject found improvement in their FLACC score.Figure 1
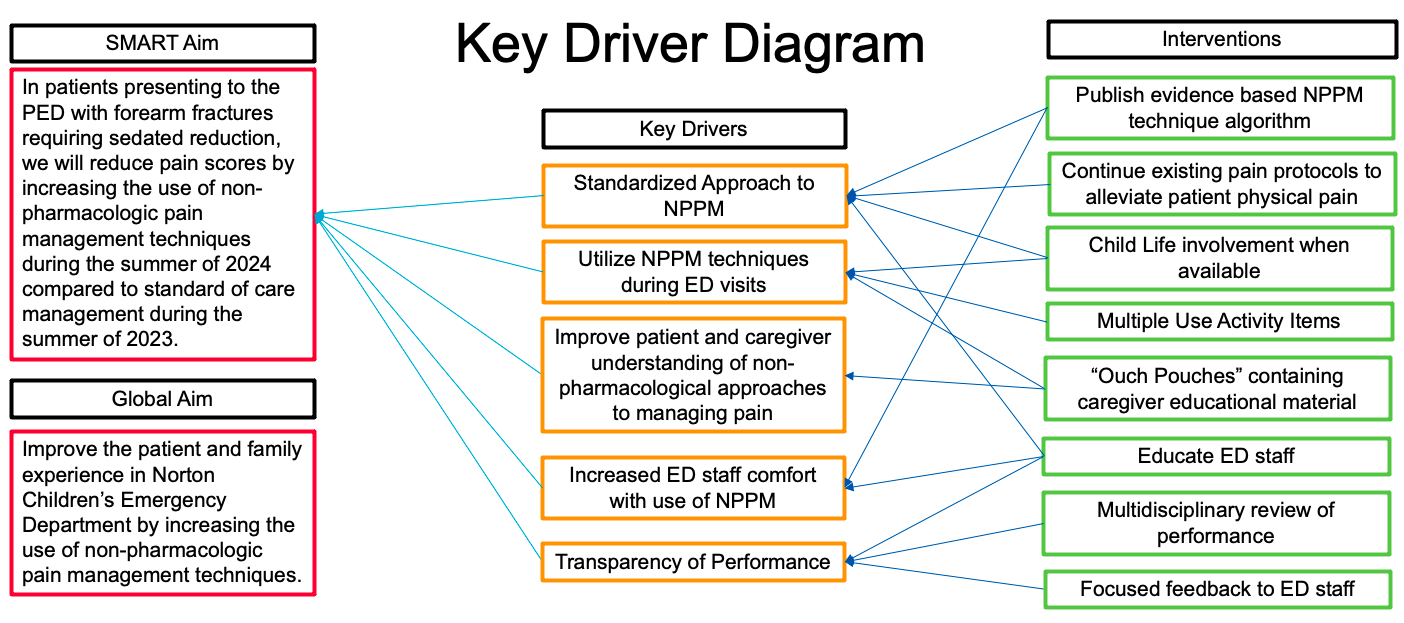 Study Design Key Driver Diagram.
Study Design Key Driver Diagram.Figure 2
.png) Non-Pharmacologic Pain Management Algorithm.
Non-Pharmacologic Pain Management Algorithm.Table 1
.jpg) Multivariate binomial regression predicting if a subject found improvement in their FLACC score.
Multivariate binomial regression predicting if a subject found improvement in their FLACC score.
