Emergency Medicine 10
Session: Emergency Medicine 10
518 - Personal and Neighborhood-level Social Determinants and Mental Health Revisits at U.S. Pediatric Emergency Departments
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 518.6267
Anna McGinty. Cushing, Children's Hospital Los Angeles, Los Angeles, CA, United States; Pradip P. Chaudhari, Children's Hospital Los Angeles, Los Angeles, CA, United States; Amy West, Children's Hospital Los Angeles, Los Angeles, CA, United States
- AC
Anna McGinty Cushing, MD (she/her/hers)
Pediatric Emergency Medicine Physician
Children's Hospital Los Angeles
Los Angeles, California, United States
Presenting Author(s)
Background: Pediatric mental health (MH) emergency department (ED) visits are increasing. Understanding predictors of MH ED revisits is important for risk stratification and targeting interventions. In a prior study, we found public insurance and higher Child Opportunity Index (COI), a composite measure of neighborhood educational, health and environmental, and socioeconomic opportunity, were both associated with MH ED revisit. These disparate findings raise questions about the role of personal compared to neighborhood-level social determinants of health in MH ED utilization.
Objective: Our objectives were to (1) evaluate the association between COI and MH ED revisits for children with public compared to private insurance and (2) determine overall visit, patient, and hospital level predictors associated with MH ED revisits by insurance type.
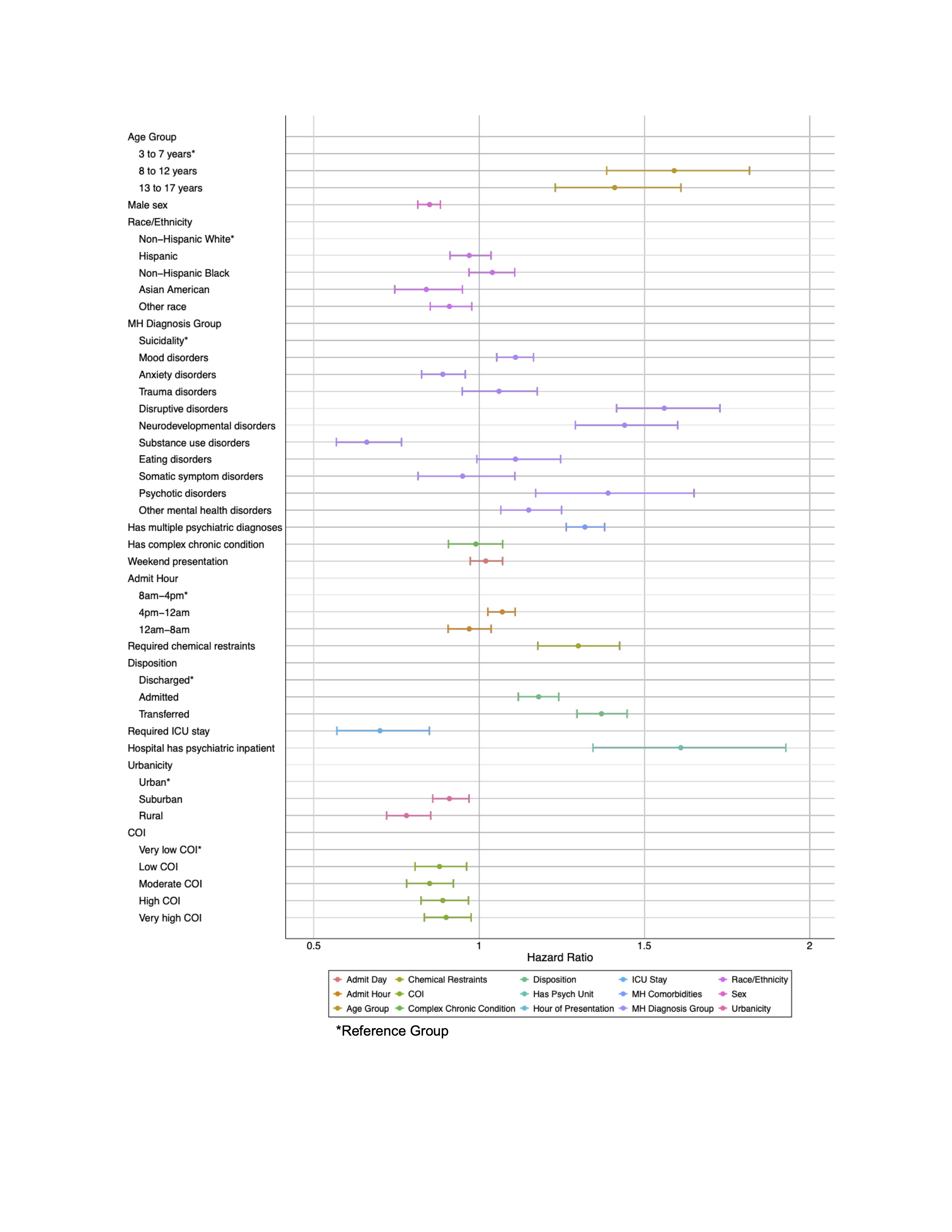
Design/Methods: We performed a cross-sectional study of children 3 to 17 years with public or private insurance who had a MH ED visit at 38 U.S. children’s hospitals from January 2021 - December 2023. Data were obtained from the Pediatric Health Information System. Our primary outcome was MH ED revisit within 180 days of the patient’s index MH ED visit. We analyzed patients by insurance type. We assessed univariate association between COI and time to MH ED revisit and then derived separate multivariable Cox Proportional Hazards Regression models using the first index visit for each patient.
Results: We included 184,931 patients with an MH ED visit during the study, of whom 53.6% (99,147) had public insurance. Children with both public and private insurance were majority female, age 13-17 years, and lived in urban areas (Table 1). There were differences in race/ethnicity by insurance type. Of included patients, 14.7% (n=27,117) had a MH ED revisit within 180 days. For children with both public and private insurance, higher COI was associated with MH ED revisit in univariate analysis. In a multivariable model, higher COI remained a significant predictor of revisit for children with public insurance (Hazard Ratio (HR) 1.13, 95% Confidence Interval (CI) 1.07-1.19, very high compared to very low COI). However, for children with private insurance, lower COI was associated with ED revisit (HR 0.90, 95% CI 0.83,0.98, very high compared to very low COI).
Conclusion(s): We identified differences in the association between COI and MH ED revisit by insurance type. Further work is needed to understand the specific components of COI that impact MH ED revisits and how this intersects with receipt of MH care outside of the ED setting.
Table 1. Demographics of Included Patients
.jpg)
Figure 1. Predictors of MH ED Revisits for Children with Public Insurance
.jpg)
Figure 2. Predictors of MH ED Revisits for Children with Private Insurance