Neonatal Pulmonology - Clinical 3: Non-invasive and Invasive Ventilation
Session: Neonatal Pulmonology - Clinical 3: Non-invasive and Invasive Ventilation
327 - Effect of Nasal Continuous Positive Airway Pressure (nCPAP) Vs Non-Invasive Positive Pressure Ventilation (NIPPV) On Diaphragm Electrical Activity (Edi) In Very Low Birth Weight (VLBW) Preterm Infants
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 327.4985
Maher Shahroor, Sunnybrook Health Sciences Center, Toronto, ON, Canada; Patti A. Schurr, Sunnybrook Health Sciences, Toronto, ON, Canada; Giselle WS. Lai, Sunnybrook Health Sciences centre, Toronto, ON, Canada; Norman Comtois, Home, Scarborough, ON, Canada; Elizabeth Asztalos, University of Toronto Temerty Faculty of Medicine, Toronto, ON, Canada; Christer Sinderby, Unity Health Toronto, York, ON, Canada; Eugene Ng, University of Toronto Temerty Faculty of Medicine, Toronto, ON, Canada; Jennifer Beck, UnityHealthToronto, Toronto, ON, Canada; Michael S. Dunn, University of Toronto Temerty Faculty of Medicine, Toronto, ON, Canada
- MS
Maher Shahroor, MD
Neonatologist
Sunnybrook Health Sciences Center
Toronto, Ontario, Canada
Presenting Author(s)
Background: Various non-invasive respiratory support strategies are used to prevent endotracheal intubation, and chronic lung disease in preterm infants. Two systematic reviews in 2023 showed that NIPPV is superior to nCPAP in reducing need for intubation within 6 hours from birth and extubation failure in preterm infants. In practice, the mean airway pressure (MAP) set in nCPAP is most often lower than the MAP set in NIPPV, which may explain the apparent inferiority of nCPAP. Measurement of Electrical diaphragmatic activity (Edi) can be used to assess infants’ neural breathing patterns and work of breathing when receiving respiratory support with different modes and pressure settings. While Edi minimum (min) reflects the residual diaphragmatic effort used to maintain functional residual capacity, Edi peak reflects effort exerted to generate an adequate tidal breath.
Objective: To determine whether using nCPAP with MAP (CPAP+) equivalent to the NIPPV MAP in VLBW preterm infants provides similar respiratory support to NIPPV as assessed by Edi measurements.
Design/Methods: Stable Preterm infants on nCPAP (5-8cmH2O, FiO2 < 0.35) were randomized in a crossover design to receive 2 hours of support with NIPPV, standard CPAP, and CPAP+ (Fig 1, Table 1). Only the order of the modes was randomized (Fig 1). An Edi catheter (Getinge®) was inserted for continuous Edi measurement; the final 20 minutes of each 2-hour epoch were analyzed. We used standard short binasal prongs ‘Fisher & Paykel®’ during the study.
Results: 24 infants with median (range) gestational age 25 (24-27) weeks and birth weight 802 (725-918) g enrolled. At the time of enrolment median postmenstrual age 31 (28-36) weeks and weight 1265 (1044-1553) g. As in Fig 2, transitioning from standard CPAP to CPAP+ significantly decreased Edi min, peak, and delta values. However, this pattern was not observed when transitioning from standard CPAP to NIPPV or from NIPPV to CPAP+. The maximum FiO2 requirements remained stable across the 3 modes with mean (SD) values of 0.27 (0.05), 0.25 (0.04), 0.24 (0.04), respectively (p=0.77). Similarly, mean (SD) of TCO2 were 52 (7.8), 52 (7.7), 52 (7.6), respectively (p=0.99). No safety concerns.
Conclusion(s): In this cohort of stable preterm infants, transitioning from standard to higher CPAP (CPAP+) significantly reduced the Edi measurements indicating improved respiratory support. This was not observed when switching between CPAP and NIPPV or NIPPV to CPAP+, likely due to non-synchronization of NIPPV. This suggests that CPAP may provide equal or superior respiratory support than non-synchronized NIPPV when providing equivalent MAP.
Table 1: Conversion scheme from Standard CPAP to NIPPV, and from NIPPV to nCPAP to provide equivalent Mean Airway Pressure (MAP)
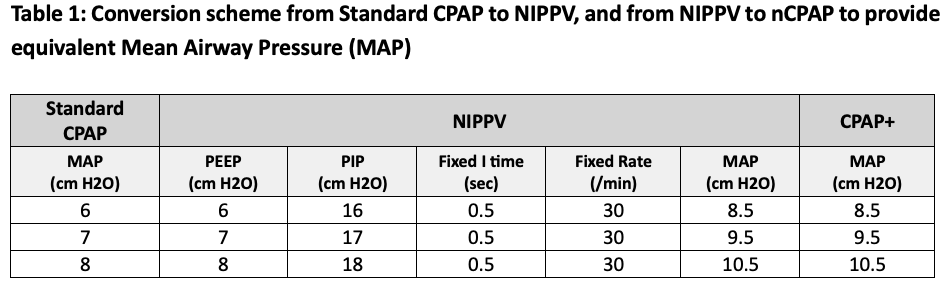
Figure 1: Randomization and intervention groups with overview of the study procedure
.png)
Figure 2: *Edi Minimum, Peak, and Delta across CPAP, CPAP+, and NIPPV Groups
.png)

