Neonatal/Infant Resuscitation 4
Session: Neonatal/Infant Resuscitation 4
396 - Comparison of Neonatal and Pediatric Resuscitation Algorithms in the Ovine Model
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 396.4094
Evan M. Giusto, UC Davis Health, Sacramento, CA, United States; Michelle J. Lim, University of California, Sacramento, CA, United States; Deepika Sankaran, University of California Davis Children's Hospital, Sacramento, CA, United States; Erin Riley, University of California, Davis, School of Medicine, Redding, CA, United States; Rebecca Valdez, University of California Davis, Davis, CA, United States; Amy Lesneski, University of California, Davis, School of Medicine, Davis, CA, United States; Victoria Hammitt, University of California, Davis, School of Medicine, Sacramento, CA, United States; Jessa Rose A. Li, University of California Davis Children's Hospital, Sacramento, CA, United States; Payam Vali, University of California, Davis, School of Medicine, sacramento, CA, United States; Satyan Lakshminrusimha, UC Davis, Sacramento, CA, United States
.jpg)
Evan M. Giusto, MSN (he/him/his)
Neonatal Nurse Practitioner
UC Davis Health
Sacramento, California, United States
Presenting Author(s)
Background: Resuscitation guidelines in pediatrics are based on the Neonatal Resuscitation Program (NRP) in the delivery room and immediate neonatal period and Pediatric Advanced Life Support (PALS) in older children. Achieving and maintaining expertise in both NRP and PALS can be challenging for prehospital providers and community emergency departments. While NRP focuses on transitional neonatal physiology and respiratory failure, PALS is more complex in nature, comprising advanced resuscitation for a broader range of cardiopulmonary events including non-perfusing dysrhythmias. The complexity of congenital conditions cared for in the NICU is increasing, as well as the upper limits of the age of convalescent infants. Further, the respiratory and hemodynamic effects of resuscitating an asphyxiated newborn with fluid-filled lungs and an open ductus in the delivery room with PALS is unknown.
Objective: Compare resuscitation with PALS to NRP in a newborn ovine model of hypoxia-induced cardiac arrest.
Design/Methods: Time-dated term fetuses were asphyxiated by umbilical cord occlusion until asystole and delivered. 12 lambs were randomized to be resuscitated with NRP or PALS (in-hospital cardiac arrest) algorithm. The NRP code leader had a background in neonatology, and the PALS code leader had a background in pediatric critical care.
Results: There was no difference in baseline characteristics (Table 1). All lambs achieved return of spontaneous circulation (ROSC) after one dose of epinephrine. Time to ROSC was the same between groups: mean (standard deviation) of 4.6 minutes (0.39) with NRP and 4.8 minutes (0.20) with PALS; p-value = 0.41. One lamb randomized to PALS went into pulseless ventricular tachycardia after ROSC and was successfully defibrillated with 4J/kg (an initial shock of 2J/kg was unsuccessful).
Ventilation was more effective with NRP compared to PALS with significantly lower PaCO2 although values were similar at ROSC (Figure 1a). PaO2 was higher in NRP lambs 2 minutes into resuscitation, but the same by 4 minutes (Figure 1b). Blood pressure was higher in the first minute of resuscitation with lambs resuscitated with PALS but similar thereafter (Figure 2).
Conclusion(s): In the setting of perinatal asphyxia, both NRP and PALS resuscitation algorithms had similar time to and frequency of ROSC. Gas exchange was transiently better in lambs randomized to NRP. Non-perfusing ventricular tachycardia was encountered in about 8% of lambs in this model of hypoxia-induced cardiac arrest. PALS may address a broader range of cardiopulmonary conditions for ongoing arrest such as non-perfusion ventricular tachycardia.
Table 1: Baseline Characteristics and Asystole Blood Gas
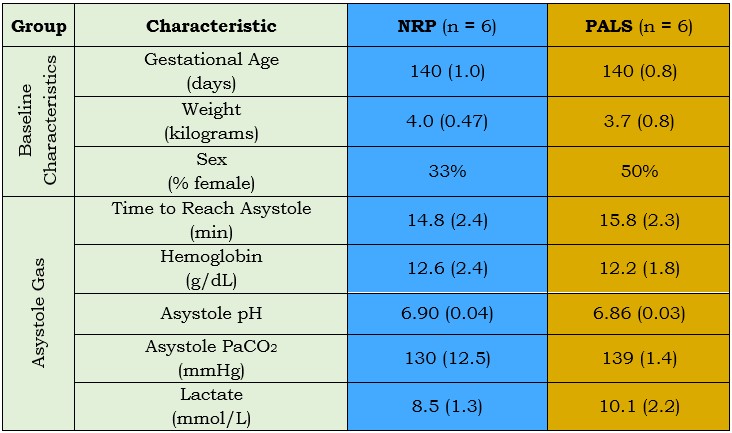 Values are mean (standard deviation)
Values are mean (standard deviation)Figure 1: Gas Exchange
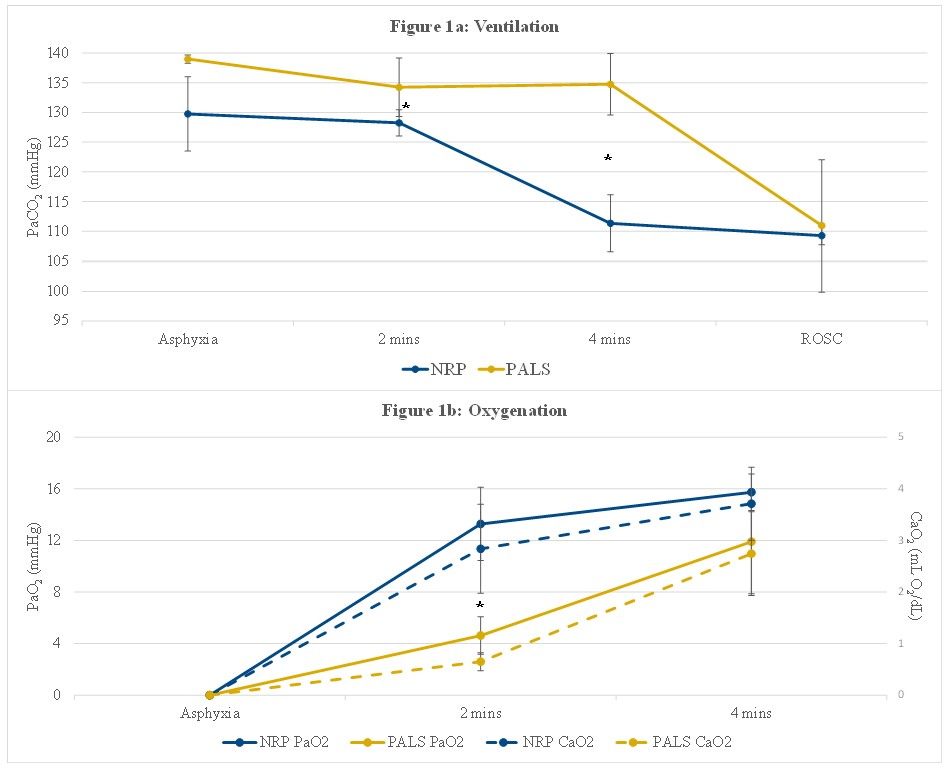 *p-value < 0.05 via unpaired t-test
*p-value < 0.05 via unpaired t-testFigure 2: Blood Pressure
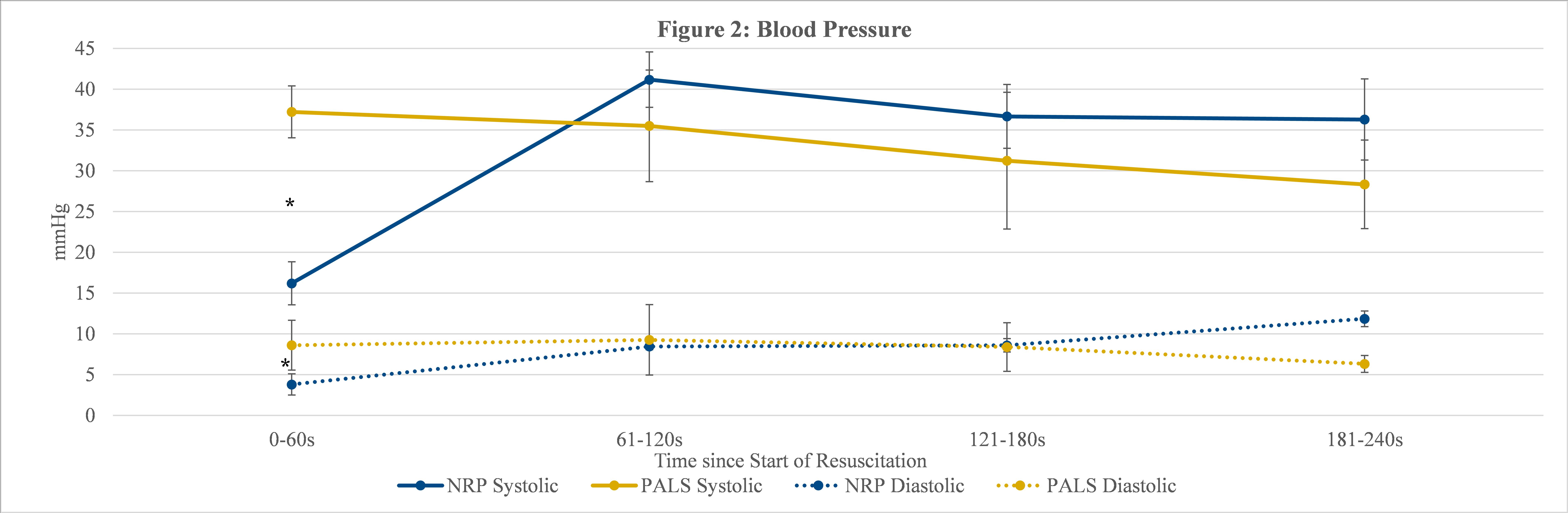 *p-value < 0.05 via unpaired t-test
*p-value < 0.05 via unpaired t-testTable 1: Baseline Characteristics and Asystole Blood Gas
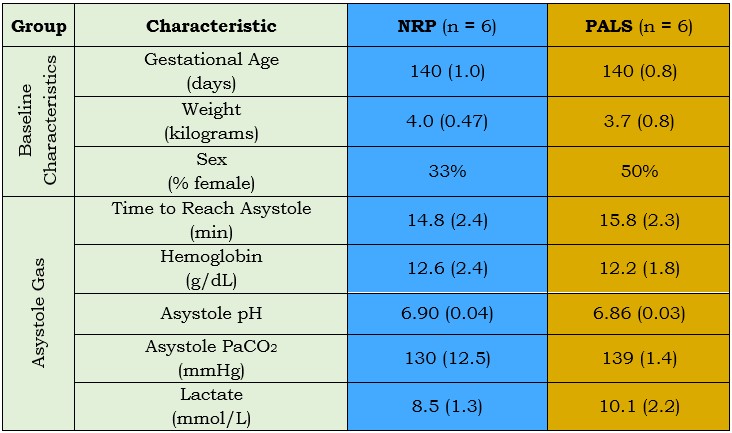 Values are mean (standard deviation)
Values are mean (standard deviation)Figure 1: Gas Exchange
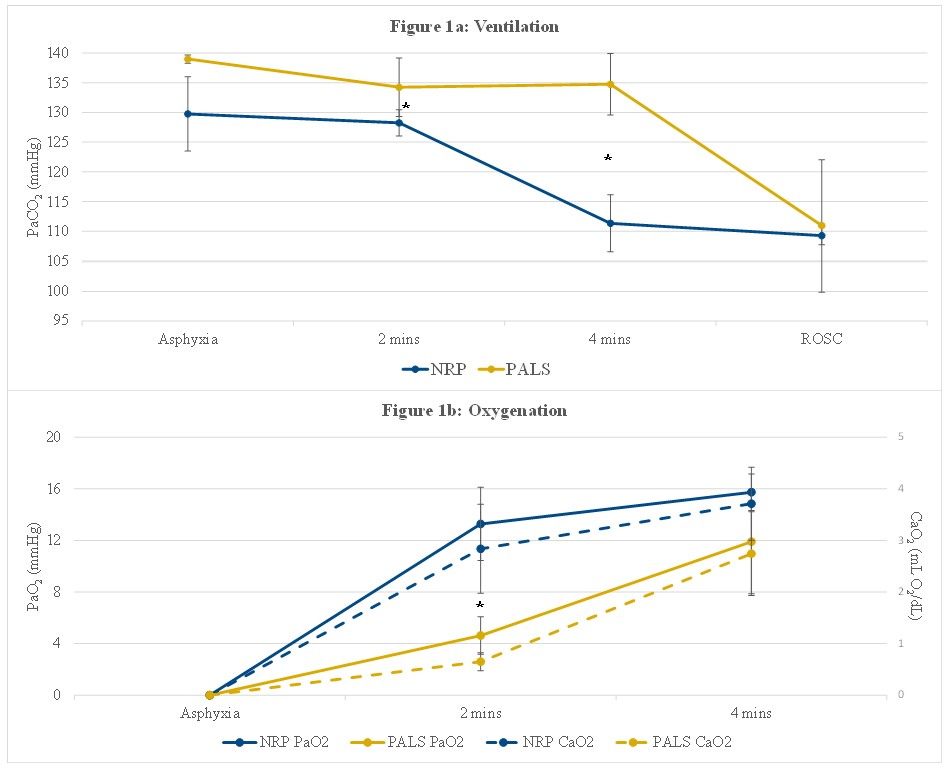 *p-value < 0.05 via unpaired t-test
*p-value < 0.05 via unpaired t-testFigure 2: Blood Pressure
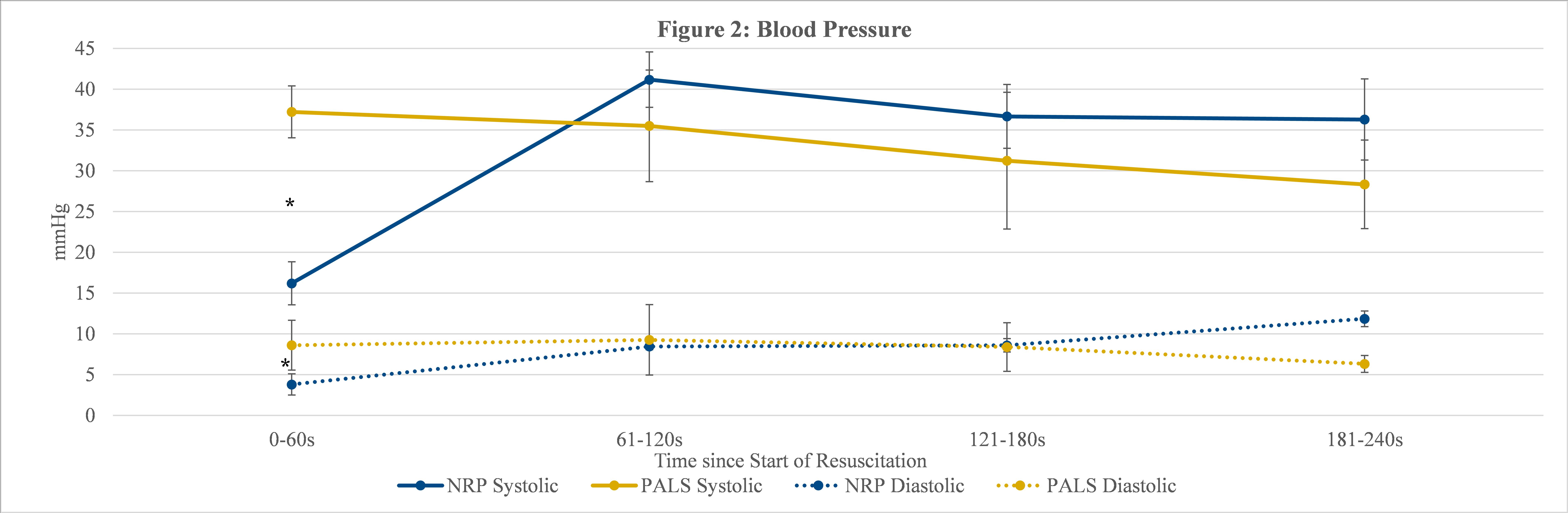 *p-value < 0.05 via unpaired t-test
*p-value < 0.05 via unpaired t-test
