Neonatal GI Physiology & NEC 4
Session: Neonatal GI Physiology & NEC 4
709 - Hospital length of stay among infants with jejunal or ileal atresia
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 709.5217
Katie Huff, Indiana University School of Medicine, Indianapolis, IN, United States; Isabella Zaniletti, IZ Statistics LLC, Tampa, FL, United States; Kera McNelis, Emory University School of Medicine, Atlanta, GA, United States; Muralidhar Premkumar, Baylor College of Medicine, Houston, TX, United States; Daniel Robinson, Northwestern University The Feinberg School of Medicine, Chicago, IL, United States; Jae H. Kim, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Abeer Azzuqa, UPMC Childrens Hospital of Pittsburgh, Pittsburgh, PA, United States; Alan P. Ladd, Indiana University, Indianapolis, IN, United States; Carl H. Coghill, UAB, Birmingham, AL, United States; Patricia W. Denning, Emory University School of Medicine, Atlanta, GA, United States; Theresa Grover, University of Colorado, Aurora, CO, United States; Michael A. Padula, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States; Karna Murthy, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Pritha Nayak, UTSW, Dallas, TX, United States
- KH
Katie Huff, MD, MS (she/her/hers)
Assistant Professor of Clinical Pediatrics
Indiana University School of Medicine
Indianapolis, Indiana, United States
Presenting Author(s)
Background: Surgical and nutritional management of small intestine atresias correlate with length of stay (LOS) in single center studies. How these variables impact short-term outcomes in a multicenter cohort is uncertain.
Objective: Our primary objective was to estimate the risk-adjusted LOS in infants with jejunal (JA) or ileal atresia (IA). Our secondary objective was to determine variability in risk-adjusted LOS between individual centers.
Design/Methods: We conducted a retrospective cohort study including infants with JA or IA treated from 2010-22 using the Children's Hospitals Neonatal Database (CHND). The Children’s Hospital National Consortium includes 49 level 4 neonatal intensive care units (NICU) across the U.S. and Canada who contribute patient data to the CHND about initial NICU hospitalization. Exclusion criteria included other gastrointestinal anomalies, highly morbid conditions (e.g., diaphragmatic hernia, necrotizing enterocolitis totalis), metabolic disorders, and incomplete records. The primary outcome was hospital LOS in survivors; the main exposure was center of care. Generalized linear multivariate modeling estimated associations between patient and clinical characteristics and LOS. Center was treated as a fixed effect; p< 0.05 was used for significance.
Results: There were 1134 and 808 infants with JA and IA, respectively. Table 1 outlines cohort information including demographic data and morbidities. Mortality was low (JA: 2.5%; IA 1.9%) and the median age of first surgery was 3 days [IQR 2,4] for JA and 4 days [IQR 2,7] for IA. The unadjusted, median LOS in survivors showed variation between hospitals (JA: 5.9 [IQR 3.7,11.1] weeks; IA: 4.6 [IQR 2.4,12.1] weeks). Risk-adjusted LOS showed 4-fold differences for JA (6.6 to 33 weeks) and 7-fold variations for IA (1.7 to 14.5 weeks; p< 0.001 for both) in multivariable analyses (Table 2). Graphically, individual centers’ estimates are reported using fixed effects modeling (Figure 1).
Conclusion(s): After adjusting for patient and clinical care characteristics, striking differences were observed in risk-adjusted LOS between hospitals for infants with JA or IA. Because surgical repairs occurred soon after birth, efforts to understand post-operative care, promotion of bowel motility/feeding tolerance, and growth will be the focus of future qualitative queries to counsel families and potentially reduce LOS for these affected infants. Further data is needed to prospectively understand if the modifiable risk factors identified in our model could be used to decrease the LOS for infants with JA or IA.
Table 1: Cohort characteristics for both jejunal and ileal atresia.
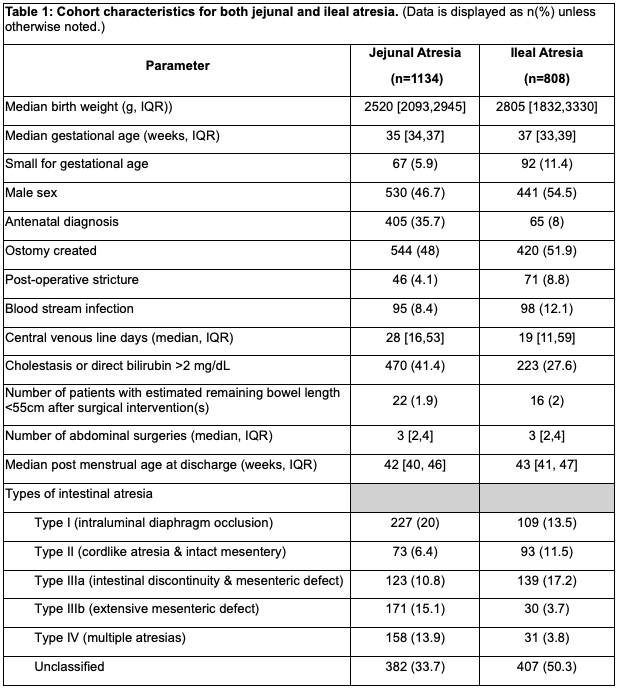 (Data is displayed as n(%) unless otherwise noted.)
(Data is displayed as n(%) unless otherwise noted.)Table 2: Multivariable analysis predicting length of stay, adjusted for center.
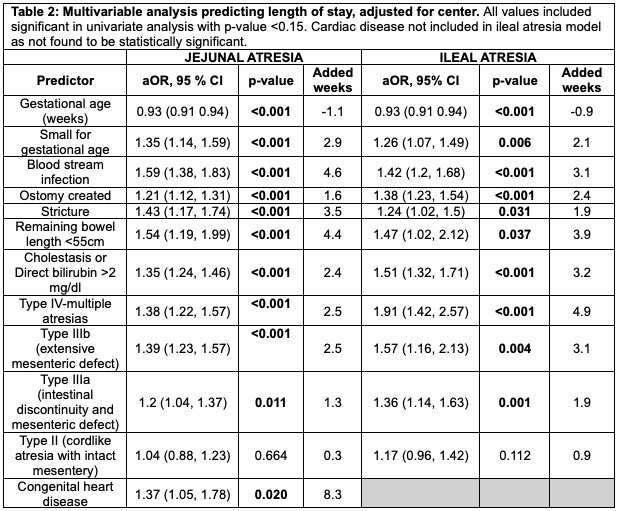 All values included significant in univariate analysis with p-value <0.15. Cardiac disease not included in ileal atresia model as not found to be statistically significant.
All values included significant in univariate analysis with p-value <0.15. Cardiac disease not included in ileal atresia model as not found to be statistically significant.Figure 1: Inter-center differences in adjusted LOS variation for surviving infants with jejunal or ileal atresia.
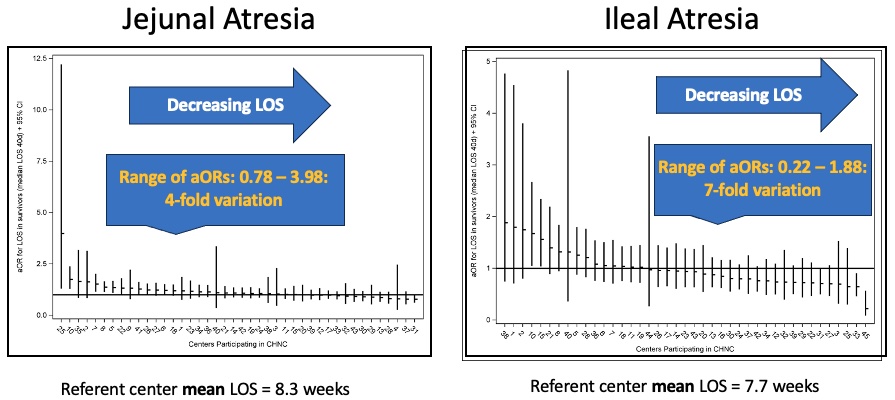 Each line represents an individual center adjusted odds ratio and 95% confidence interval. Blinded center codes represent the same hospital on each graph panel. After adjusting for the variables in Table 2, risk-adjusted LOS demonstrated striking variations between hospitals (JA: 6.6 to 33 weeks; IA: 1.7 to 14.5; p<0.001 for both).
Each line represents an individual center adjusted odds ratio and 95% confidence interval. Blinded center codes represent the same hospital on each graph panel. After adjusting for the variables in Table 2, risk-adjusted LOS demonstrated striking variations between hospitals (JA: 6.6 to 33 weeks; IA: 1.7 to 14.5; p<0.001 for both).
