Neonatal Fetal Nutrition & Metabolism 4
Session: Neonatal Fetal Nutrition & Metabolism 4
648 - Longitudinal Growth Patterns by Gestational Age Among Extremely Preterm Infants from NICU Hospitalization to 12 Months Post-Discharge
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 648.5783
Margaret L.. Ong, Brigham and Women's Hospital, Boston, MA, United States; Hunter L. Pepin, Brigham and Women's Hospital, Boston, MA, United States; Deirdre M. Ellard, Brigham and Women's Hospital, Boston, MA, United States; Ava L. Cho, University of Chicago Division of the Biological Sciences The Pritzker School of Medicine, Moultonborough, NH, United States; Saharnaz Talebiyan, Brigham and Women’s Hospital, Boston, MA, United States; Melissa Woythaler, Brigham and Women's Hospital, Boston, MA, United States; Elizabeth YORK. Flanigan, Elizabeth, Westford, MA, United States; Elisa A. Abdulhayoglu, Brigham & Women's Hospital, Boston MA, MA, United States; Laura B.. Bernardini, Brigham and Women's Hospital and Harvard Medical School, Boston, MA, United States; Mandy Belfort, Harvard Medical School, Boston, MA, United States

Margaret L. Ong, MD, MPH (she/her/hers)
Neonatologist
Brigham and Women's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Extremely preterm infants born < 28 weeks gestational age (GA), especially those born ≤24 weeks’ GA, are nutritionally vulnerable due to immature digestive and motility function and altered nutrient accretion, exacerbated by ongoing critical illness. With a current focus on improving the survival of infants born ≤24 weeks’ GA, it is critical to examine their growth, both during neonatal intensive care unit (NICU) hospitalization and after discharge.
Objective: Among extremely preterm infants: 1) describe anthropometric measurements in NICU and post-discharge through 12 months’ corrected age; 2) compare these outcomes between infants born ≤24 weeks’ vs 25-27 weeks’ GA and 3) assess the impact of clinical illness on growth differences between groups
Design/Methods: We studied 284 infants born < 28 weeks GA who remained admitted to the NICU on day 28 in a single academic center. We collected anthropometric measurements and z-scores at birth, day 28, 35 weeks post-menstrual age (PMA), NICU discharge, and post-discharge visits (initial, 4 and 12 month) from the medical record, using Olsen and WHO (for corrected age) references for ≤41 weeks and >41 weeks PMA, respectively. To quantify differences in outcomes between infants of GA ≤24 vs >24 weeks, we used median regression, adjusting for size for GA at birth and multiple gestation (Model 1). We also adjusted for comorbidity count (Model 2), hypothesizing that this would attenuate associations between GA and outcomes.
Results: Median (range) GA was 26.3 (22.3-27.9) weeks [Table 1]. In the NICU, median z-scores were negative across GA, indicating size less than the fetal reference. We observed the lowest z-scores among those born ≤24 weeks’ [Table 2]. In Model 1, infants born ≤24 weeks had lower weight, length, and head circumference z-scores at day 28 (beta (95% CI): -0.22 (-0.43, -0.01), -0.29 (-0.49,-0.09), -0.27 (-0.53, -0.01), respectively) and PMA 35 weeks (-0.26 (-0.48, -0.04), -0.59, (-0.84, -0.34), -0.43 (-0.70, -0.16), respectively) compared with infants born >24 weeks. Differences in length z-score persisted to 4-month follow-up [Table 3]. Additional adjustment for clinical illness (Model 2) did not substantially attenuate associations.
Conclusion(s): Our findings indicate substantial linear growth stunting during NICU hospitalization among infants born ≤24 weeks’ GA compared to more mature 25-27 week infants, which persisted through 4 months’ corrected age. Critical illness did not fully account for differences in growth by GA, suggesting the importance of other aspects of extremely preterm birth leading to growth failure that warrant further attention.
Table 1: Participant Characteristics
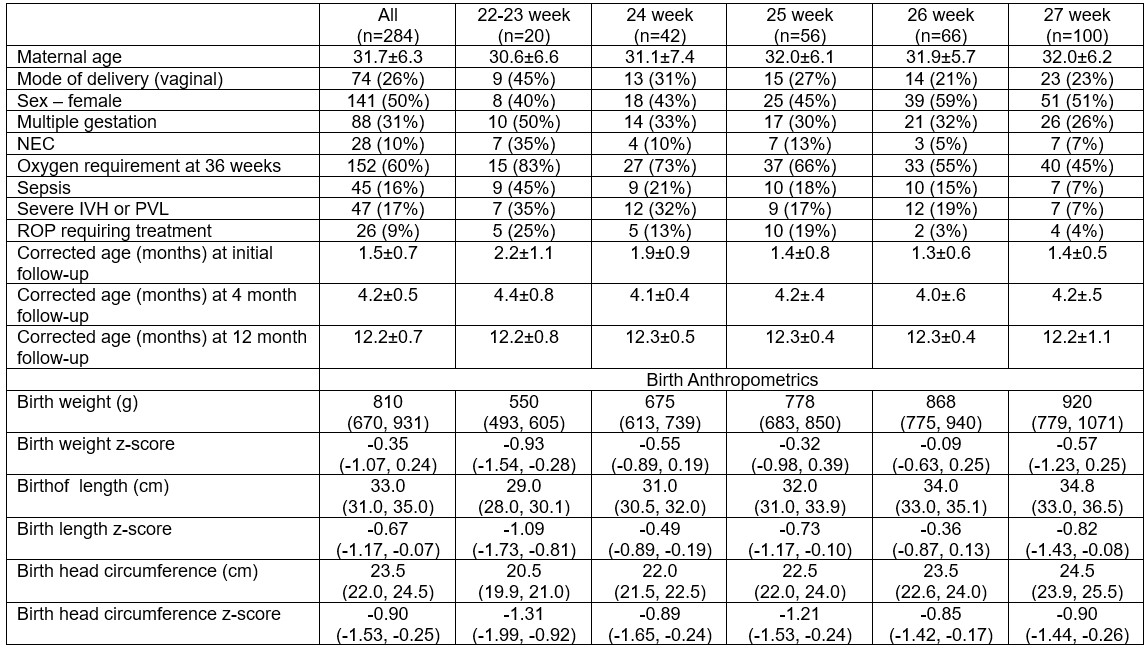 Demographic data are represented as mean±SD or n (% of gestational age category n). Anthropometric z-scores are presented as median (IQR). NEC: necrotizing enterocolitis. Sepsis: early/late onset bacterial or fungal sepsis. Severe IVH or PVL: grade III-IV intraventricular hemorrhage or periventricular leukomalacia. ROP: retinopathy of prematurity. Birth z-scores were derived using Olsen reference. Note: birth anthropometric z-scores for 22-23 week group do not capture <23 week on Olsen reference.
Demographic data are represented as mean±SD or n (% of gestational age category n). Anthropometric z-scores are presented as median (IQR). NEC: necrotizing enterocolitis. Sepsis: early/late onset bacterial or fungal sepsis. Severe IVH or PVL: grade III-IV intraventricular hemorrhage or periventricular leukomalacia. ROP: retinopathy of prematurity. Birth z-scores were derived using Olsen reference. Note: birth anthropometric z-scores for 22-23 week group do not capture <23 week on Olsen reference. Table 2. Anthropometric Z-scores during NICU Hospitalization and Post-Discharge Follow-up among Extremely Preterm Infants by Gestational Age
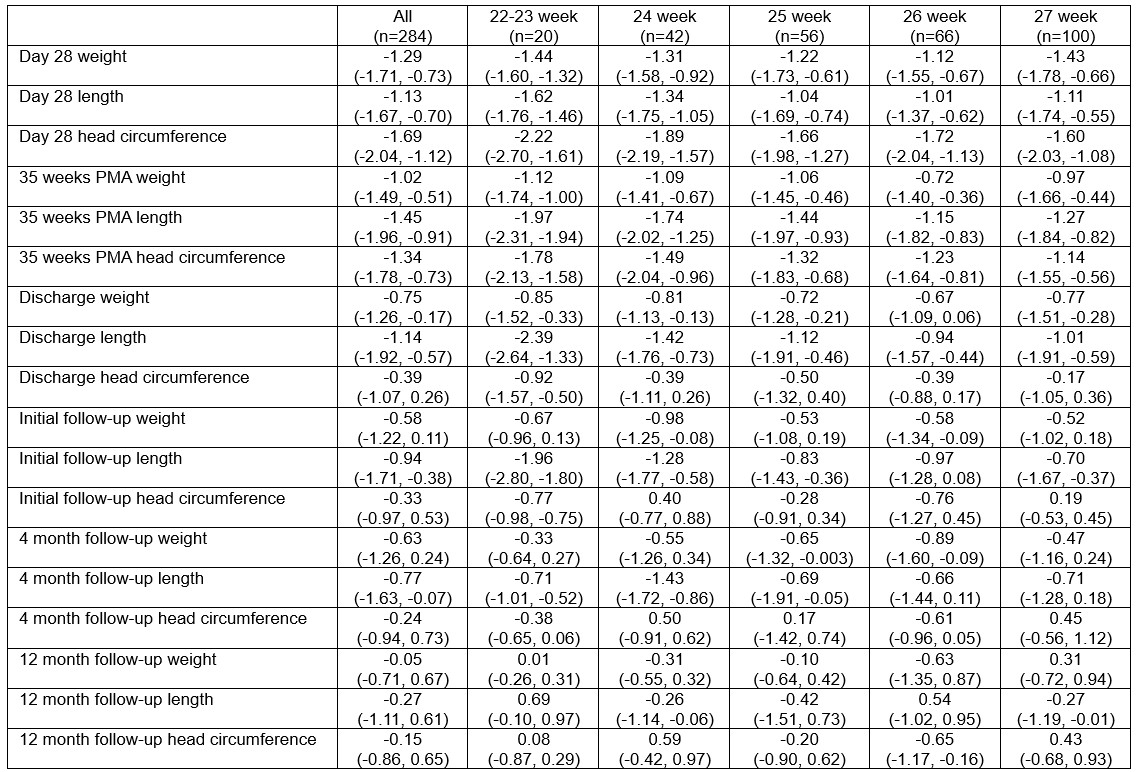 Data are represented as median (IQR). Z-scores were derived using Olsen reference for PMA ≤41 week and WHO reference (for corrected age) for PMA >41 weeks.
Data are represented as median (IQR). Z-scores were derived using Olsen reference for PMA ≤41 week and WHO reference (for corrected age) for PMA >41 weeks. Table 3: Median Regression Models Assessing Differences in Anthropometric Outcomes Between Infants Born at ≤24 weeks vs >24 weeks Gestational Age during NICU Hospitalization through 12 Months' Corrected Age
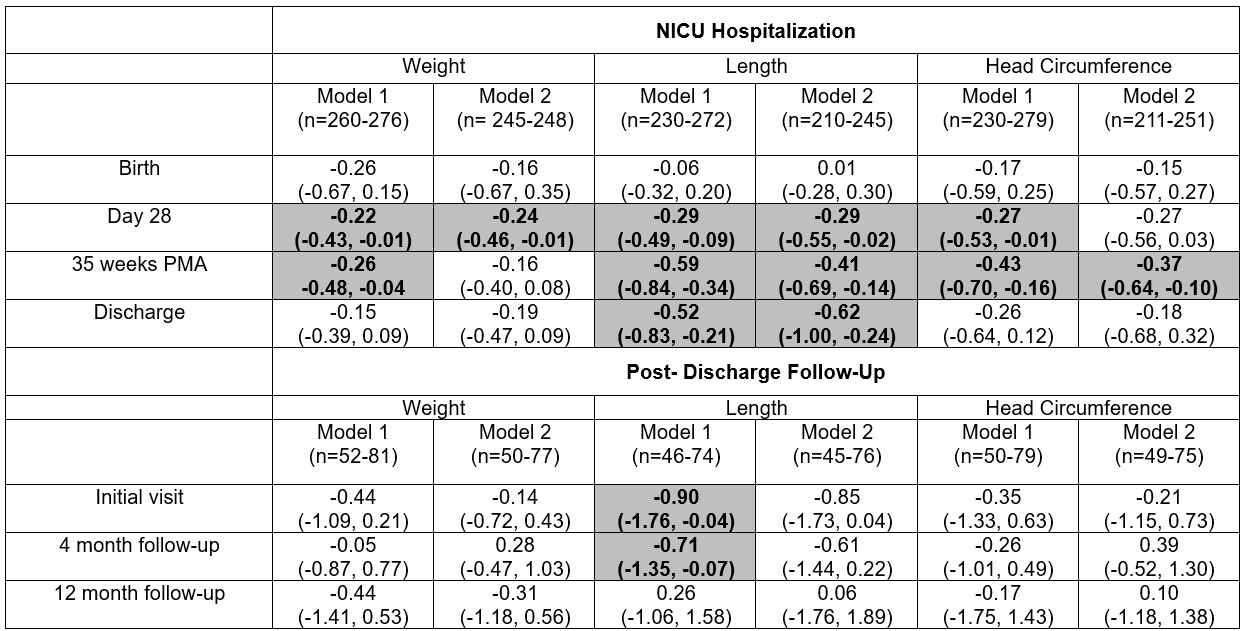 PMA: post-menstrual age. Beta estimates indicate difference in median anthropometric z-score comparing infants born ≤24 weeks gestation vs those born >24 weeks (reference). Median regression models were adjusted for covariates of interest. Model 1 adjusted for multiple gestation and size for GA at birth (small, average, or large for gestational age), except models for birth which do not adjust for birth size. Model 2 adjusted for covariates in Model 1 + comorbidity count as an indicator of clinical illness (oxygen requirement at 36 weeks, retinopathy of prematurity requiring treatment, and intraventricular hemorrhage grade III or IV or periventricular leukomalacia). Z-scores were calculated using Olsen reference for PMA ≤41 week and WHO reference (for corrected age) for PMA >41 weeks. Shaded bolded results indicate p<0.05. Note: birth anthropometric z-scores do not capture <23 week on Olsen reference.
PMA: post-menstrual age. Beta estimates indicate difference in median anthropometric z-score comparing infants born ≤24 weeks gestation vs those born >24 weeks (reference). Median regression models were adjusted for covariates of interest. Model 1 adjusted for multiple gestation and size for GA at birth (small, average, or large for gestational age), except models for birth which do not adjust for birth size. Model 2 adjusted for covariates in Model 1 + comorbidity count as an indicator of clinical illness (oxygen requirement at 36 weeks, retinopathy of prematurity requiring treatment, and intraventricular hemorrhage grade III or IV or periventricular leukomalacia). Z-scores were calculated using Olsen reference for PMA ≤41 week and WHO reference (for corrected age) for PMA >41 weeks. Shaded bolded results indicate p<0.05. Note: birth anthropometric z-scores do not capture <23 week on Olsen reference.
