Neonatal Fetal Nutrition & Metabolism 1
Session: Neonatal Fetal Nutrition & Metabolism 1
612 - Care Of Neonates Following In-Utero Growth Restriction: A Prospective Cohort Study Exploring Neonatal Morbidity.
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 612.4140
Maria G. Alda, Mercy Hospital for Women, Caulfield East, Victoria, Australia; Maria Alda, Mercy Hospital for Women, Caulfield East, Victoria, Australia; Amanda Wood, Deakin university, Burwood, Victoria, Australia; Teresa M. MacDonald, The University of Melbourne, Melbourne, Victoria, Australia; Julia K. Charlton, University of British Columbia Faculty of Medicine, Vancouver, BC, Canada

Maria G. Alda, MD (she/her/hers)
Neonatologist
Mercy Hospital for Women
Melbourne, Victoria, Australia
Presenting Author(s)
Background: Fetal growth restriction (FGR) is associated with an increased risk of neonatal mortality and morbidity and can often coexist with prematurity. Distinguishing the impacts of prematurity versus FGR has proven difficult. A comprehensive evaluation of neonatal trajectories and attributable risks is yet to be conducted.
Objective: To compare neonatal morbidities in Small-for Gestational-Age (SGA) preterm infants to those of gestation-matched and birthweight-matched controls.
Design/Methods: Prospective cohort study of premature infants born between 24+0 and 36+6 weeks’ gestation admitted to an Australian tertiary neonatal nursery between April 2023 and February 2024. SGA infants (birthweight < 10th centile on Gestation Related Optimal Weight chart) were recruited and matched with well-grown (birthweight ≥10th centile) infants according to their gestation, birthweight, and sex. We recorded neonatal clinical data, including growth and neonatal morbidities. Growth trajectory was measured as change in z-scores using Fenton Charts from birth to discharge.
Results: 150 preterm infants were included in the study (56 SGA; 54 controls in each group). SGA infants were more likely to experience hypothermia and necrotizing enterocolitis (NEC) than both control groups. SGA infants were more likely to experience hypoglycaemia compared to birthweight-matched controls. In contrast, intraventricular haemorrhage (IVH) was significantly more prevalent among birthweight-matched controls compared to the SGA infants. SGA infants recovered to their birthweight (day 8) significantly faster than controls (day 11 p < 0.0002 for both control groups) but demonstrated lower changes in weight z-scores (tables 1 & 2). There were no significant differences in length of stay, or requirements for respiratory or inotropic support between cohorts.
Conclusion(s): Being SGA is an independent risk factor for the neonatal complications of hypothermia and NEC beyond the risks incurred by being premature, or of low birthweight despite being well-grown for gestation. Being SGA is also a greater risk factor for hypoglycaemia than being low birthweight, but appropriate-for-gestational-age. In contrast, lower gestation at birth is a significant risk factor for IVH, rather than birthweight centile. Preterm SGA infants have a different neonatal growth trajectory compared to their well-grown preterm infants. These data may inform expectations of growth for SGA neonates.
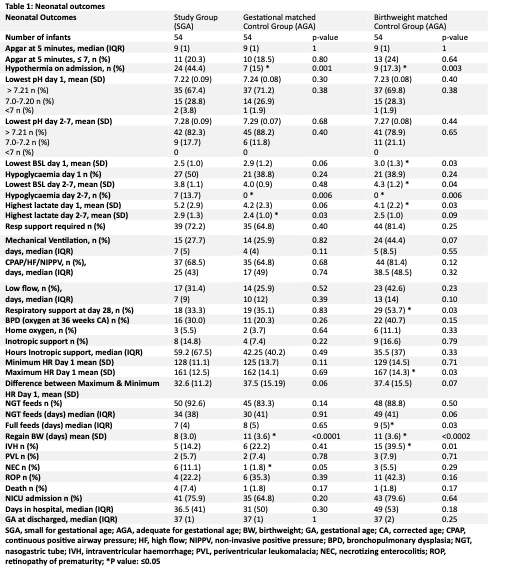
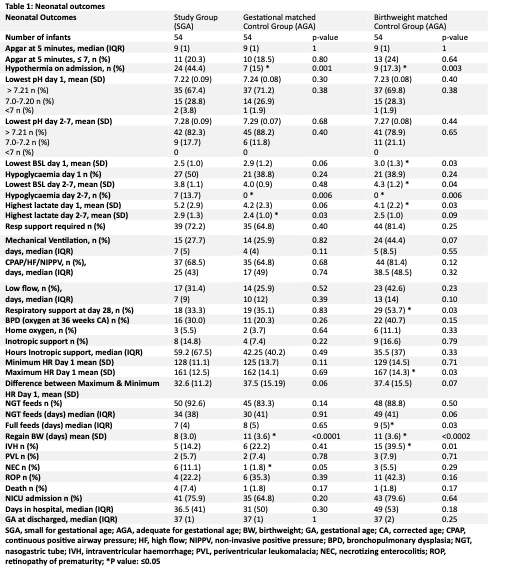
Neonatal Outcomes
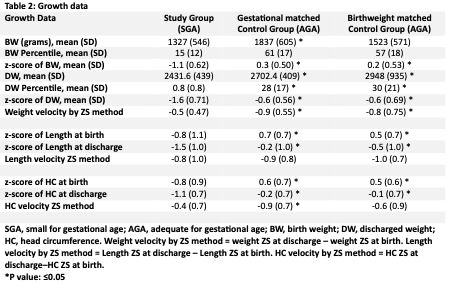
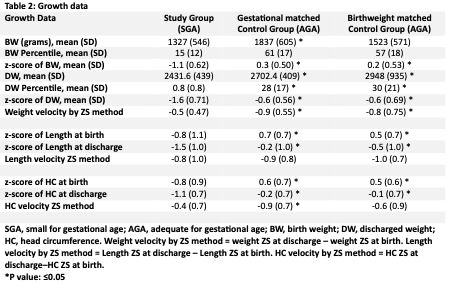
Growth data
Neonatal Outcomes
Growth data