Public Health & Prevention 4
Session: Public Health & Prevention 4
802 - Participant and staff perspectives on nutrition education in WIC to inform the development of an early obesity prevention program for Latino families in a post-COVID era
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 802.5995
Nirupa Galagedera, Cohen Children's Medical Center, Bayside, NY, United States; Mary Jo Messito, New York University Grossman School of Medicine, New York, NY, United States; Elsy R. Escobar, Northwell Pediatrics Center, AMITYVILLE, NY, United States; Emely Sanchez, Cohen Children's Medical Center, Uniondale, NY, United States; Victoria E.. Chaparro, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Everett, MA, United States; Sophia Jan, Cohen Children's Medical Center of Northwell Health, New Hyde Park, NY, United States; Carol Duh-Leong, Hassenfeld Children's Hospital at NYU Langone, New York, NY, United States; Rachel S. Gross, New York University Grossman School of Medicine, New York, NY, United States; Michelle W. Katzow, Cohen Children's Medical Center, Northwell Health, New Hyde Park, NY, United States

Nirupa Galagedera, MD (she/her/hers)
Resident Physician
Cohen Children's Medical Center, Northwell Health
Bayside, New York, United States
Presenting Author(s)
Background: The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) provides food benefits, formal nutrition instruction, breastfeeding support, and community referrals to over half of all families in the United States. This makes it an ideal platform for obesity prevention programming, however, there is little published data to inform the development of such programs in a post-pandemic context. There is also a dearth of evidence on the experience of Latino mothers and children, who are most at risk for obesity and its sequelae, and comprise the highest WIC enrollment rates, underscoring the need to better understand and optimize their experiences.
Objective: To characterize WIC participant and staff perceptions of nutrition education strategies after the onset of the COVID pandemic to inform the development of an early obesity prevention program for Latino families in WIC.
Design/Methods: We conducted 40 semi-structured interviews with Latina WIC participants and 5 focus groups with WIC staff from 2022 – 2024.Data were audio-recorded, transcribed, and translated to English as necessary. We used a mixed deductive and inductive approach to conduct a thematic analysis.
Results: Table 1 describes demographic characteristics of participants in each stakeholder group. Table 2 describes key themes that emerged, namely facilitators and barriers to nutrition education, with representative quotes from each stakeholder group for each of the primary functions of WIC. Suggestions from WIC participants and staff for a future early obesity prevention program for Latino families largely overlapped and converged into three major areas: structures to maintain continuity, participant-specific content, accommodation of obstacles detailed in Table 3.
Conclusion(s): Utilizing focus groups and semi-structured interviews of WIC maternal participants and staff across New York state, we identified facilitators, barriers, and suggestions for improvement to nutrition education delivery via WIC following COVID-19 related pandemic changes. Future steps must be taken to create a participant-driven, longitudinal, early obesity prevention program that accommodates current programming hindrances, including cultural mismatch, inadequate time, insufficient access, and desire for stimulating content.
Table 1: Sample characteristics of 40 WIC participants and 13 WIC staff
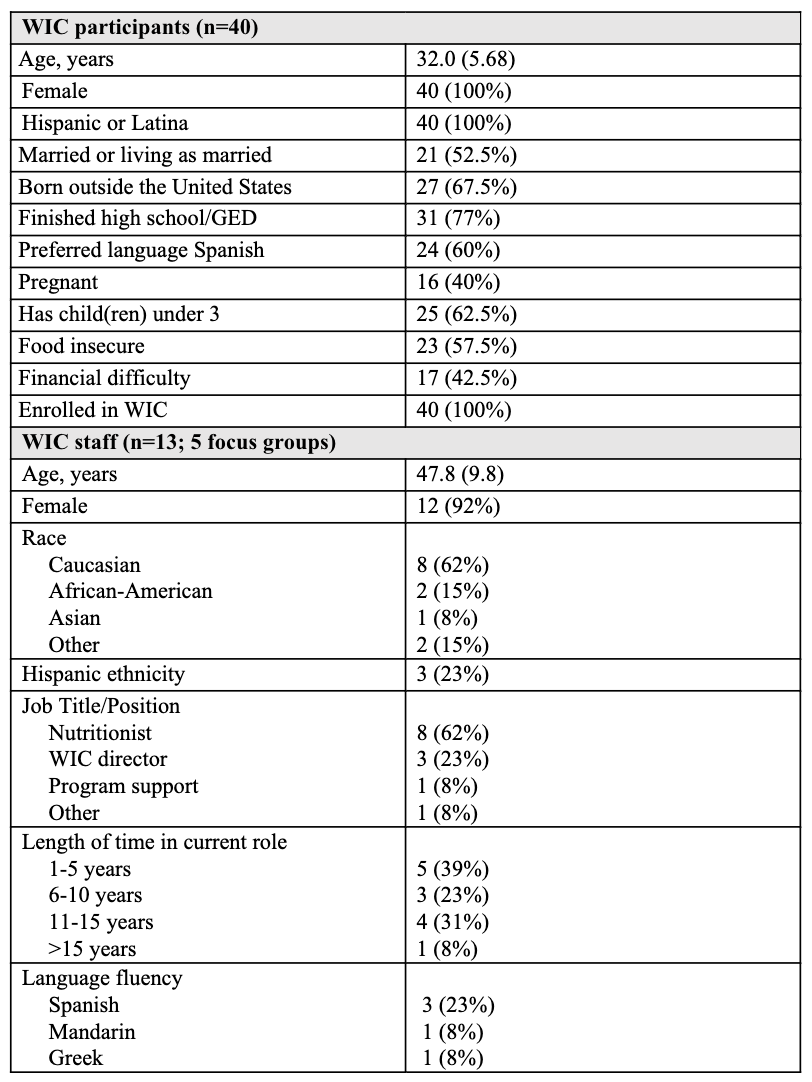
Table 2: Facilitators and barriers to nutrition education in WIC after the onset of the COVID-19 pandemic as perceived by WIC participants and staff
.png)
Table 3: Suggestions for WIC to improve nutrition education delivery for Latino mothers and children
.png)

