Neonatal General 11
Session: Neonatal General 11
422 - Accessibility of Neonatal Point of Care Ultrasound (POCUS) Training through a Credentialed Pathway: A Survey of Australian and New Zealand Neonatal Clinicians
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 422.3709
Penny Pei Lee Kee, Western Health, Melbourne, Victoria, Australia; Arun Sett, Western Health, Melbourne, Victoria, Australia; Asiyath Rasheed, Children's Hospital, Melbourne, Victoria, Australia; Niranjan A W. Thomas, Joan Kirner Women's and Children's at Sunshine Hospital, Western Health, St Albans, Victoria, Australia
- PK
Penny Pei Lee Kee, MBBS, BMedSci, CCPU, FRACP, MClinEd
Consultant Neonatologist
Western Health
Melbourne, Victoria, Australia
Presenting Author(s)
Background: The benefits of using point of care ultrasound (POCUS) in the neonatal intensive care unit (NICU) are well established, and many countries are working towards a credentialed pathway for POCUS training. The Australian and New Zealand model for training and accreditation was developed in 2009 and is the first of such certification available internationally. Despite a credentialed program being available in the last 15 years, the number of certified neonatal clinicians have only increased from 32 to 42 in the last 10 years. There is a paucity of data on the interest in uptake and accessibility of training to neonatal clinicians.
Objective: This survey aimed to (i) characterise the exposure to POCUS training amongst neonatal clinicians, (ii) explore the availability and utility of POCUS in the NICUs, (iii) identify the perceived barriers and enablers in accessing training, and (iv) explore the preferred training models amongst neonatal clinicians.
Design/Methods: An online questionnaire was designed and distributed through the Australian and New Zealand Neonatal Network (ANZNN) mailing list in May 2024. The mailing list consists of NICU directors, neonatologists, and trainees registered with the network.
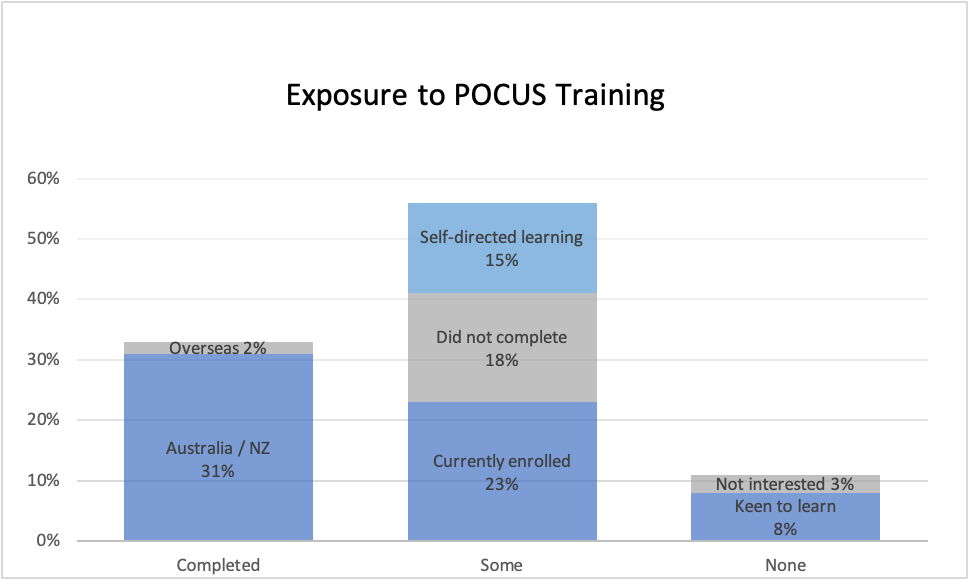
Results: A total of 132 (47%) responses were received. 88 (67%) were from consultant neonatologists, and the rest trainees. 44 (33%) have completed POCUS training, 74 (56%) have had some exposure to training, and 14 (11%) have had none. 129 (98%) work in a NICU where POCUS service is available, with 57 (43%) available around the clock, and the rest available ad hoc (43%) or during business hours only (12%). The main enablers of training include clinician perception that POCUS skills would improve diagnostic accuracy and reduce procedure related complications. The main barriers include a lack of protected teaching time, supervisors and a local curriculum, as well as concerns regarding patient misdiagnosis and maintenance of proficiency. 95 (72%) felt that POCUS training should be included in the neonatal/perinatal specialist training curriculum, and 75 (57%) indicated they would be willing to extend their training time to train in POCUS.
Conclusion(s): Neonatal clinicians recognise the importance of POCUS training and its application to improve patient outcomes. However, there are significant barriers limiting access to training. The results of this survey will help inform curriculum design and educational strategies that can lead to wider implementation of training.
Exposure to POCUS Training
Availability of POCUS service in the NICU
.png)

