Public Health & Prevention 4
Session: Public Health & Prevention 4
793 - RSV hospitalization rates among first-season infants residing in remote communities
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 793.6357
Allison Watts, University of British Columbia Faculty of Medicine, Vancouver, BC, Canada; Marina Viñeta Páramo, University of British Columbia Faculty of Medicine, Vancouver, BC, Canada; Hind Sbihi, BC Centre for Disease Control, Vancouver, BC, Canada; Pascal Lavoie, University of British Columbia, Vancouver, BC, Canada

Allison Watts, PhD (she/her/hers)
Project Manager
University of British Columbia Faculty of Medicine
Vancouver, British Columbia, Canada
Presenting Author(s)
Background: Advisory committees recommend RSV immunization for infants entering their first viral season, prioritizing remote communities. However, we lack an understanding of the relationships between health, geographic and socioeconomic factors on disease risk.
Objective: To determine the risk of RSV hospitalizations among children in their first RSV season by community remoteness in British Columbia (BC), Canada, and the contribution of health, geographic and socioeconomic factors.
Design/Methods: Retrospective population cohort analysis of all live births in BC, Canada between Jan 2013 and April 2024 followed throughout their first RSV Season (October-March) until September 30th. Data on RSV hospitalizations (ICD-10 codes) were obtained from the BC Covid-19 Cohort, a linked administrative database. Residential community health service area was classified as metropolitan, urban, rural and remote according to BC Ministry of Health and Statistics Canada’s Index of Remoteness. Neighbourhood median household income and household size were obtained from the 2016 Canadian census. Incidence rates were expressed per 1000 person years. Mixed-effects Poisson regression was used to model the risk of RSV hospitalization by level of remoteness adjusted for sex, co-morbidities, prematurity, socioeconomic factors and clustering of individuals within communities.
Results: Among 431,597 children, there were 4,096 (0.95%) RSV-related hospitalizations. Baseline characteristics such as sex, prematurity and comorbidities were similar between groups (Table 1). The incidence of hospitalization was highest in remote communities (IR=12.6 [95%CI:8.8-17.5]), followed by rural (IR=9.9 [95%CI:9.0-10.9]), urban (IR=10.5 [95%CI:10.0-11.1]) and metropolitan (IR=7.9 [95%CI:7.5-8.3]) communities. Infants in remote communities required longer hospital stays, but fewer PICU stays, suggesting less severe infections. A significant proportion required air transport (Table 1). RSV hospitalization rate remained 63% higher in remote compared to metropolitan communities after adjustment for sex, prematurity, comorbidities, neighbourhood income and household size (Table 2).
Conclusion(s): Infants in remote communities had higher rates of RSV hospitalization independent of baseline health and socioeconomic factors. This increased risk may be explained by healthcare seeking patterns, low viral exposure or genetic/physiological differences. As RSV immunoprophylaxis is implemented it will be important to determine whether these interventions effectively prevent RSV hospitalizations in those communities.
Table 1. Differences in individual factors, socioeconomic factors and RSV hospitalizations by community remoteness
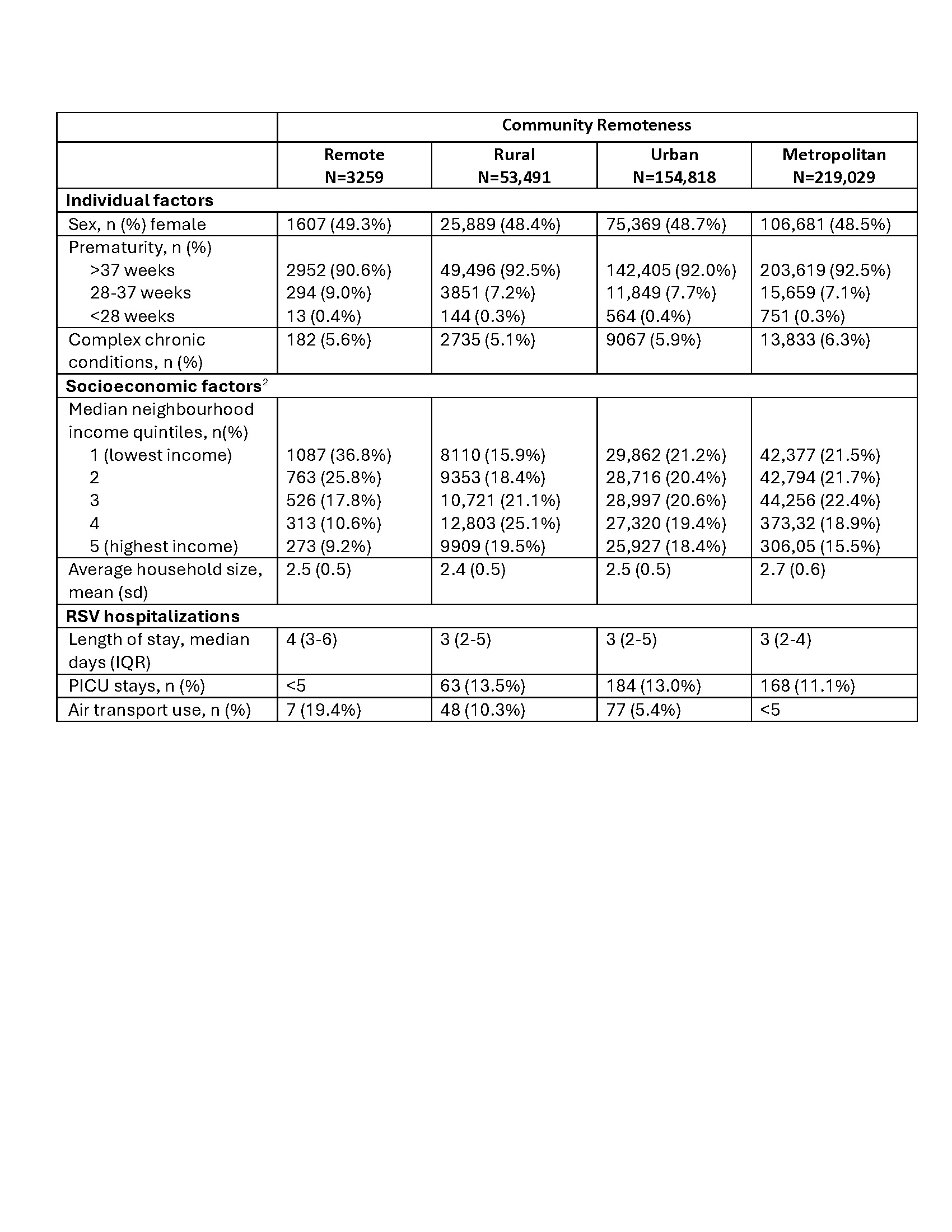 2-missing data on income and household size, respectively (n=40,286 [9.4%]; n=40,781 [9.5%] / 430,597)
2-missing data on income and household size, respectively (n=40,286 [9.4%]; n=40,781 [9.5%] / 430,597)Table 2. Relative risk of RSV hospitalization by level of community remoteness accounting for personal and socioeconomic factors.
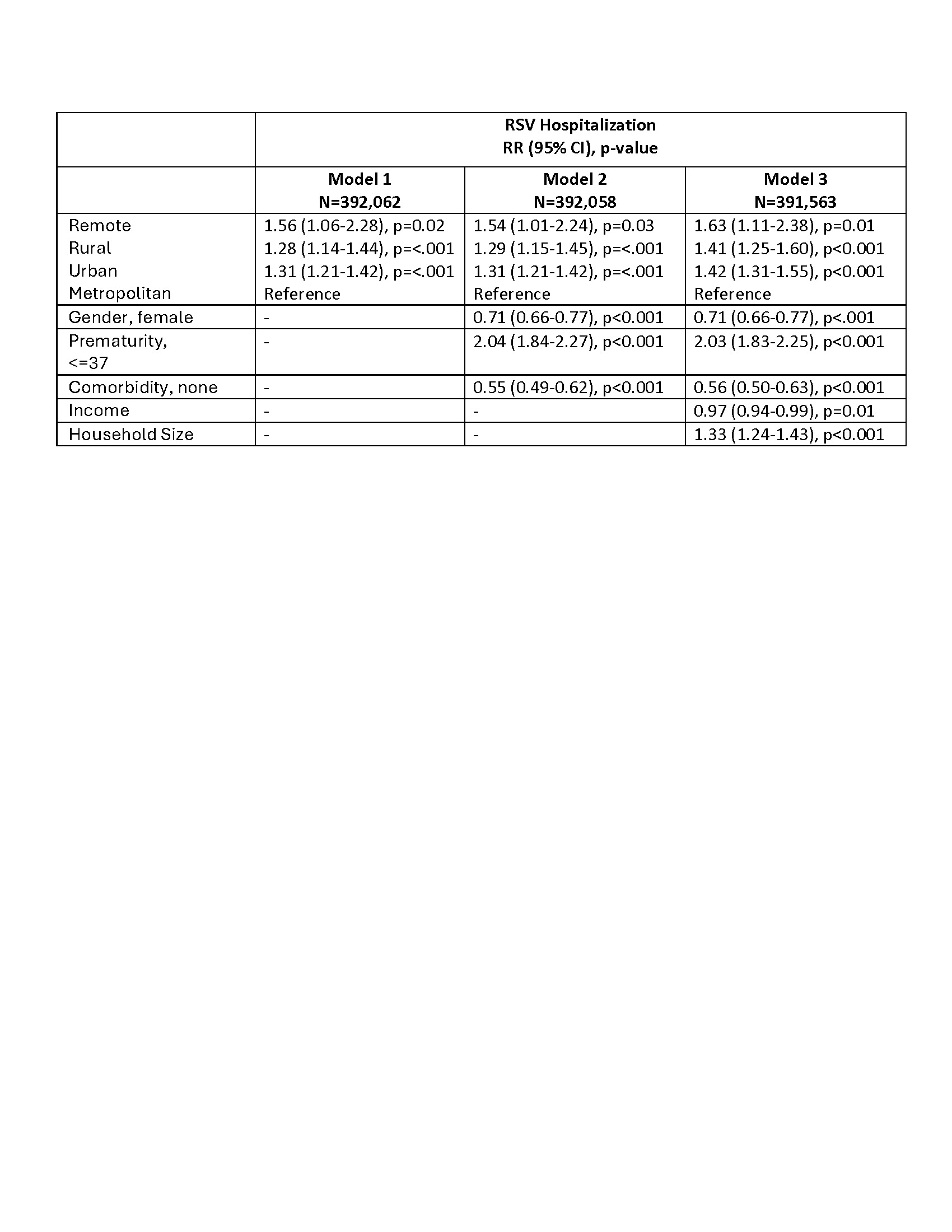 Mixed-effects Poisson regression accounting for clustering within communities
Mixed-effects Poisson regression accounting for clustering within communities
