Neonatal Fetal Nutrition & Metabolism 4
Session: Neonatal Fetal Nutrition & Metabolism 4
639 - The Metabolic Signature of term amniotic fluid is modified by maternal pre-pregnancy obesity with decreased indole and SCFA metabolites
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 639.6642
Rafael Lemus, University of Texas Southwestern Medical School, Dallas, TX, United States; Tina A. Seidu, University of Texas Southwestern Medical School, Dallas, TX, United States; Allison Kurzeja, University of Texas Southwestern Medical Center, Dallas, TX, United States; Nicole Seyfried, University of Texas Southwestern Medical School, Dallas, TX, United States; Xinying niU, UT southwestern medical center, Grapevine, TX, United States; Dongmei Lu, University of Texas Southwestern Medical School, Dallas, TX, United States; Emily Adhikari, University of Texas Southwestern Medical Center, Dallas, TX, United States; Julie Mirpuri, University of Texas Southwestern Medical School, Irving, TX, United States

Rafael Lemus, DO
Fellow
University of Texas Southwestern Medical School
Dallas, Texas, United States
Presenting Author(s)
Background: Pre-pregnancy obesity has been associated with adverse pregnancy outcomes including miscarriage, gestational diabetes, pre-eclampsia, preterm delivery, and increased infant mortality. Metabolites are present in amniotic fluid from ultrafiltration of maternal serum, produced by the microbiome and modified by diet. Metabolites, including indoles and short chain fatty acids (SCFA) are known to enhance innate immunity. Although obesity is multi-factorial, diet plays an important role. In this study, we wanted to investigate if amniotic fluid metabolites obtained at the time of term delivery are modified by maternal pre-pregnancy Body Mass Index (BMI) and maternal diet.
Objective: To compare the metabolic signature in term amniotic fluid from women with pre-pregnancy obesity and normal weight.
Design/Methods: This was a pilot study of pregnant individuals admitted to Parkland Hospital for a scheduled, term cesarean section with unruptured membranes and who were not in labor. Clear amniotic fluid samples were collected at the time of hysterotomy and stored at -80C until analysis. Pregnant individuals were divided into two different groups based on pre-pregnancy BMI: Normal ( < 25) and Obese (≥ 30). Each participant filled out a validated-Dietary Screener Questionnaire (NHANES) to identify two statistically significant dietary patterns, healthy and unhealthy. Unbiased amniotic fluid metabolomic profiling was performed by flow injection mass spectrometry. Welch's two sample t test were performed on log-transformed data with FDR correction using Benjamini-Hochberg procedure; P < .05 was considered significant. Maternal demographics and fetal anthropometrics was obtained by chart review.
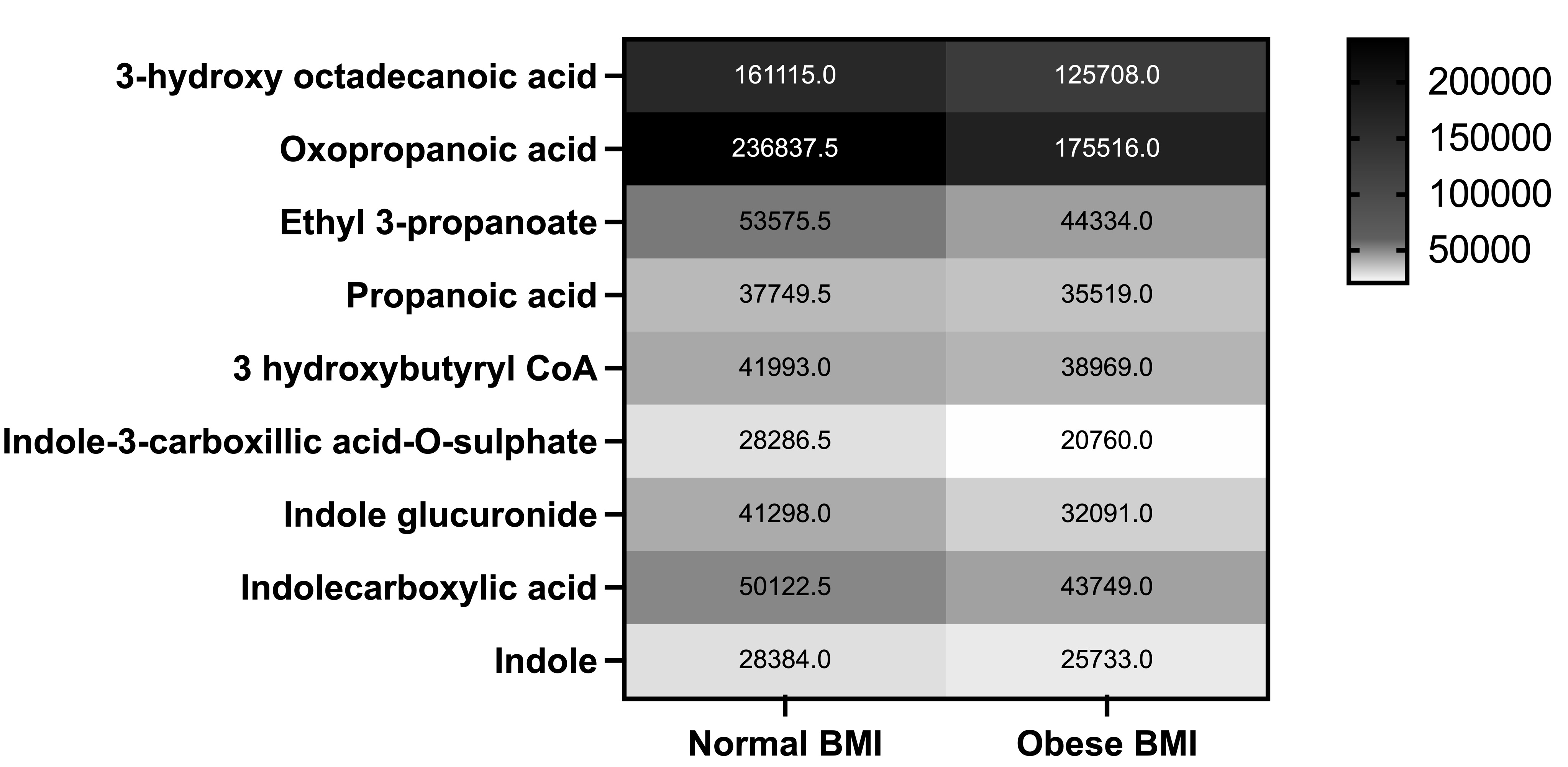
Results: 177 patients were consented, among them, 30 were from normal BMI patients and 37 from obese patients. Maternal demographics and fetal anthropometrics are presented in Table 1. Unbiased metabolomics of amniotic fluid identified 1423 unique metabolites in human amniotic fluid at time of delivery, with 287 metabolites significantly different in obese vs normal BMI. Multiple indole and SCFA metabolites were significantly diminished in the obese amniotic fluid (Figure 1). Comparison based on maternal diet and BMI status is ongoing.
Conclusion(s): Pre-pregnancy obesity decreases indole and SCFA metabolites in amniotic fluid at term. We speculate that this could modify immune priming in utero in the fetus. This potentially provides novel therapeutic supplementary options for mothers and preterm infants to enhance immunity and affect long term outcomes.
Table 1: Maternal demographics and fetal anthropometrics
.png)
Figure 1: Heatmap of statistically significant (p < 0.05) SCFA and indole metabolites comparing Obese BMI and Normal BMI expressed as average median intensity.