Neonatal Hematology & Bilirubin Metabolism 2
Session: Neonatal Hematology & Bilirubin Metabolism 2
669 - Efficacy of Treating Anemia of Prematurity with Erythropoietin Stimulating Agents (ESAs) in Very Low Birth Weight Infants
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 669.4627
Brooke N. Mangano, Metro Health Medical Center, Avon Lake, OH, United States; PRABHU S. PARIMI, Metro Health Medical Center, Clevelabd, OH, United States

Brooke N. Mangano, BS (she/her/hers)
Chester Research Scholar
Metro Health Medical Center
Avon Lake, Ohio, United States
Presenting Author(s)
Background: Very Low Birth Weight (VLBW) preterm infants experience "anemia of prematurity" after birth. This is a pronounced decline in hemoglobin (Hb) and hematocrit (Hct), with severity correlated with lower gestational age and birth weight. Frequent routine phlebotomy testing contributes to anemia in this population. Packed Red Blood Cell (PRBC) transfusions and erythropoiesis stimulating agents (ESAs) such as Epoetin alfa (EPO) are used to increase Hb and Hct levels. Previous studies have revealed risks and benefits of EPO and PRBC transfusions such as risk of retinopathy of prematurity (ROP) (Kandasamy et al., 2014), infection, or neuroprotective effects (Juul 2012).
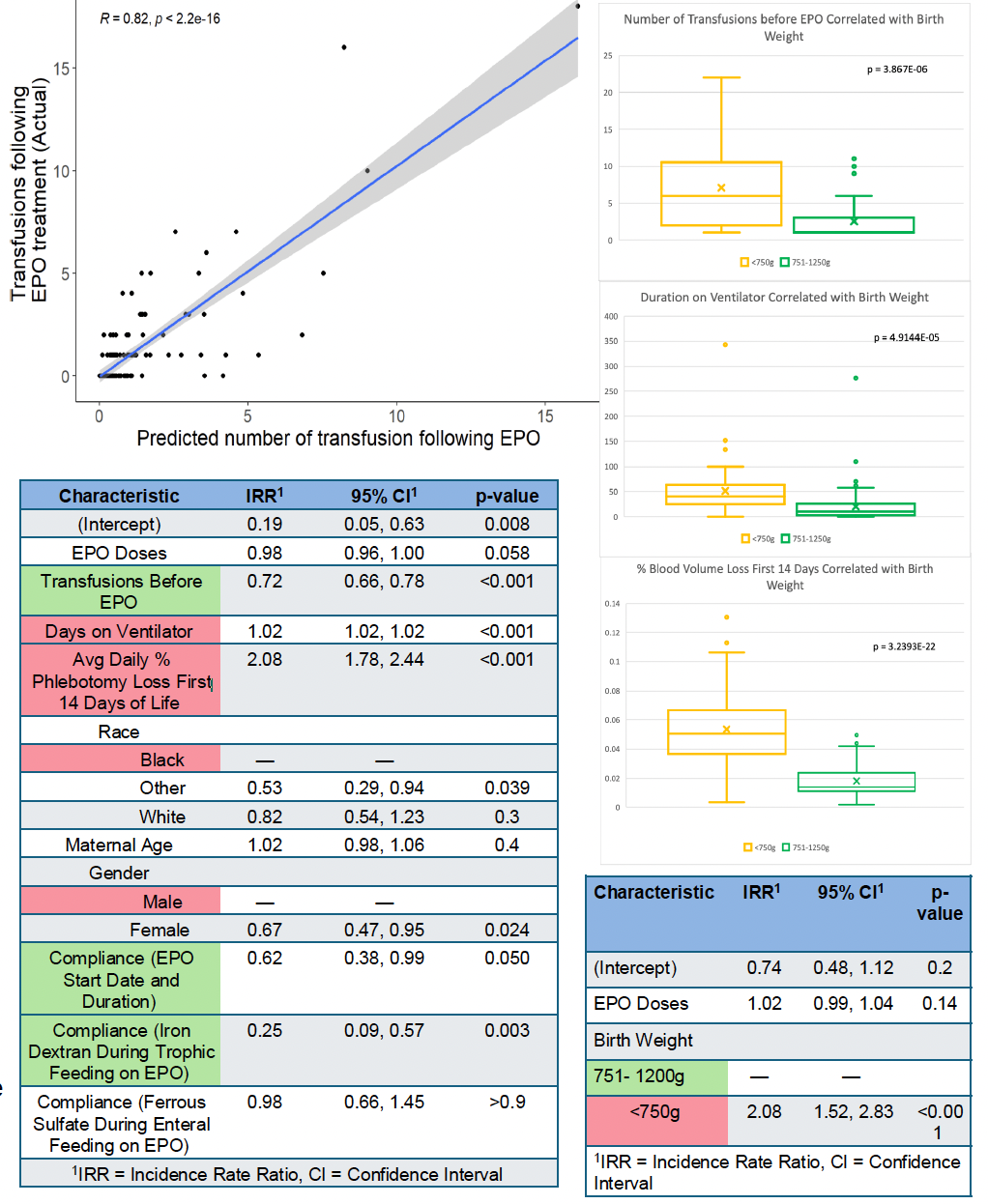
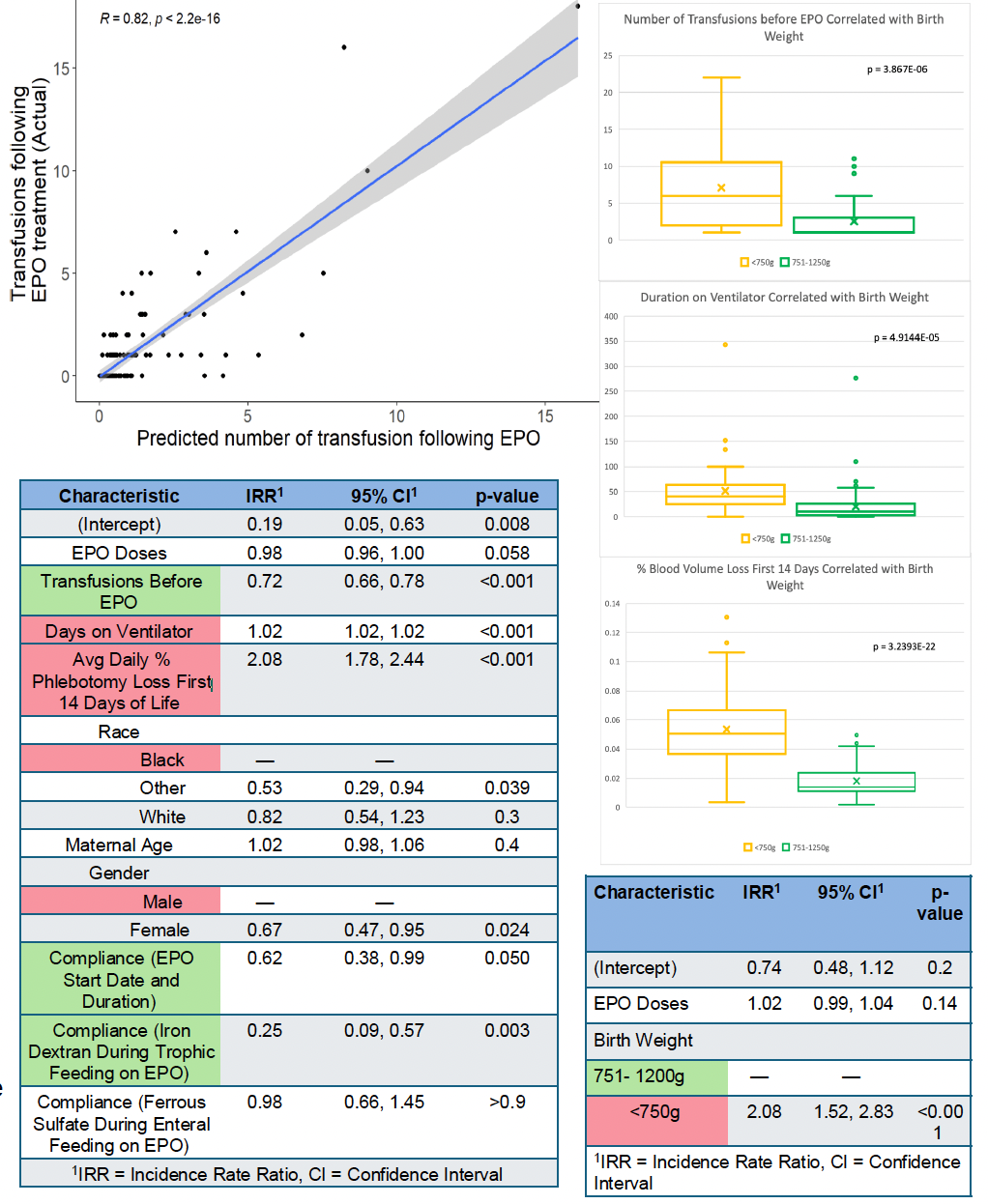
Objective: This study evaluates the degree to which EPO decreases the need for PRBC transfusions in VLBW neonates. It also identifies the risks and benefits of EPO treatment and PRBC transfusions in subsets of the population to consider optimal treatment plans. We hypothesized compliance to EPO guidelines decreases transfusions. Additionally, it is expected that a subset of more clinically severe VLBW infants are less responsive to EPO and are likely to receive multiple PRBC transfusions.
Design/Methods: A REDCap database tool was used to enter data from EPIC charts of all preterm NICU patients < 30 weeks gestational age and birth weight < 1250g from 2020-2023. Variables included demographics, birth weight, gestational age, respiratory support, course of EPO treatment, transfusion dates, and Hct/Hb data. Clinical outcome data was also collected which included ROP, bronchopulmonary dysplasia (BPD), and necrotizing enterocolitis. Data was analyzed using R.
Results: The model shows that duration of respiratory support and % phlebotomy loss are factors that decrease EPO efficacy in VLBW patients. These variables are highly correlated with birth weight. When looking at birth weight only, smaller babies are more than twice as likely to receive additional transfusions after EPO. The model also shows that more transfusions before EPO decreases transfusions after treatment. Outcomes such as ROP and BPD were more pronounced in this lower range, which could be due to EPO and/or iron supplementation.
Conclusion(s): EPO treatment decreases PRBC transfusions in VLBW infants in the upper range of very low birth weights due to less severe respiratory distress and phlebotomy loss. Results showed that necessary early transfusions in patients in the lower range of birth weights may be resolving the anemia on its own. PRBC transfusions alone as treatment in this subpopulation would avoid the risk of EPO and iron supplementation to cause adverse secondary outcomes.
Demographics and Clinical Outcomes
.png)
Variables Affecting Number of Transfusions After EPO Treatment
Demographics and Clinical Outcomes
.png)
Variables Affecting Number of Transfusions After EPO Treatment