Neonatal/Infant Resuscitation 4
Session: Neonatal/Infant Resuscitation 4
407 - Respiratory Function Monitor in First Response Training: A Feasibility Study
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 407.6461
Anneleisa S. Brimley, University of Melbourne, Sandhurst, Victoria, Australia; Elizabeth K. Baker, Royal Women's Hospital, Bellbrae, Victoria, Australia; Kate Hodgson, Royal Women’s Hospital, Parkville, Victoria, Australia; Jennifer A. Dawson, The Royal Women's Hospital, Melbourne, Victoria, Australia; Peter Davis, Royal Women's Hospital, Melbourne, Victoria, Australia; Marta Thio, The Royal Women's Hospital Melbourne, Albert Park, Victoria, Australia
- MT
Marta Thio, Doctor
Neonatal Consultant
The Royal Women's Hospital Melbourne
Albert Park, Victoria, Australia
Presenting Author(s)
Background: Face-mask ventilation during neonatal resuscitation is challenging. Mask leak is a common cause of failure to deliver effective tidal volumes. The optimal training frequency for this important skill has not been investigated thoroughly. Self-directed learning using a respiratory function monitor has the potential to establish and maintain adequate skill levels.
Objective: To investigate the feasibility of a self-directed monthly face-mask ventilation training program within a busy hospital environment. Secondary outcomes included investigating the effectiveness of the RFM in this context.
Design/Methods: A randomised controlled trial conducted at The Royal Women's Hospital, Melbourne, Australia. Clinicians were recruited from the maternity and neonatal wards. Each participant used the RFM (JunoTM) during their initial session of mannikin face mask ventilation. For the next four monthly sessions, clinicians were randomised into the intervention group (respiratory function monitor visible), or the control group (respiratory function monitor not visible). An assessment session in the final month of the study measured inflation rate, face-mask leak and tidal volume during face mask ventilation performed on a mannikin. Clinicians then completed a survey on user satisfaction with the device.
Results: Of the 62 clinicians recruited, 34% (21/62) completed all sessions. Barriers to attending included clinical workload and leave. Clinician self-assessed satisfaction with the program was high with the majority of clinicians reporting feeling more confident following the training sessions (39/46, 82%). No important differences in median mask leak, tidal volume and inflation rate were observed between groups following training (Figure 1). The intervention group demonstrated a reduction in the proportion of inflations that had a substantial leak (greater than 30%, 13.3% vs 18.7%) and a tidal volume of less than 12mL (14% vs 5%), following the training period. However, the control group had an increase in the proportion of inflations that had a leak greater than 30% (13.3% vs 18.7%) following training compared with baseline (Table 1).
Conclusion(s): Short, monthly face-mask ventilation sessions within a busy clinical environment are challenging due to clinical workload and leave. Training with a respiratory function monitor was associated with a reduction in proportion of inflations delivered with a substantial leak.
Table 1
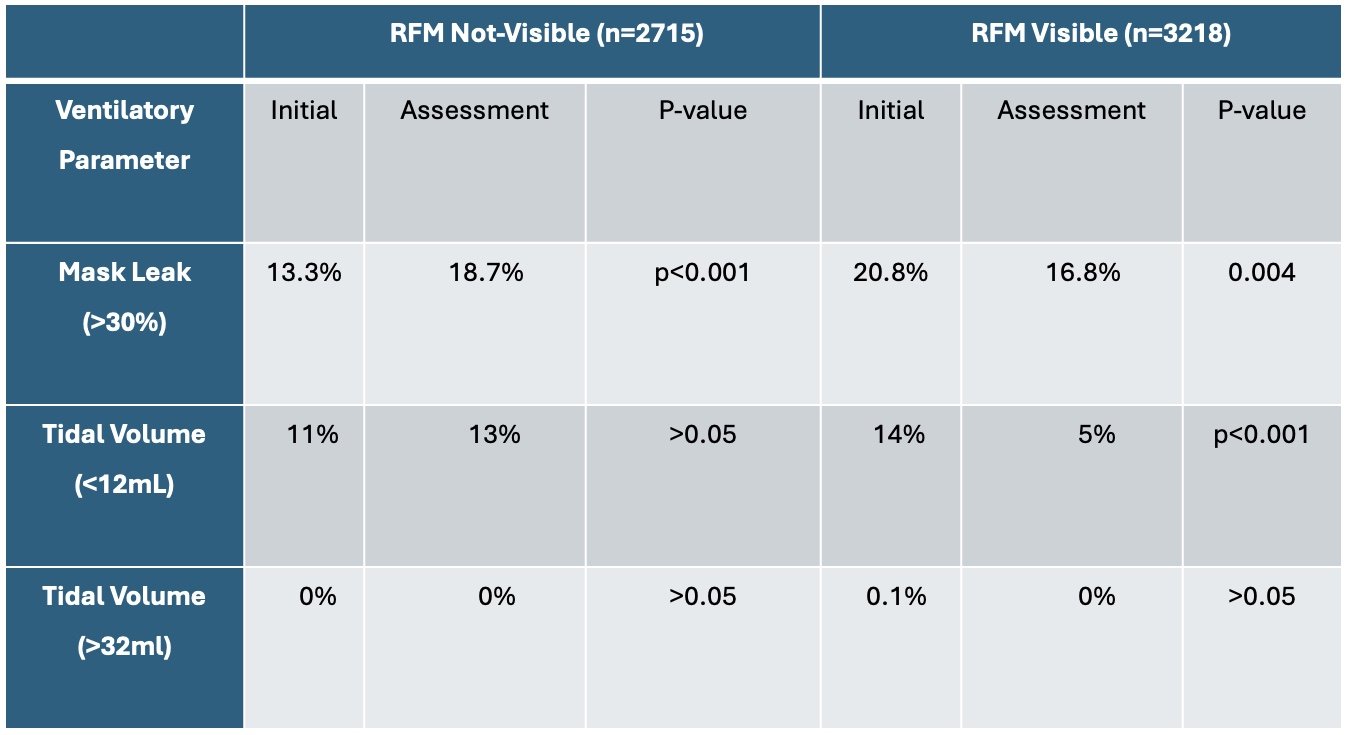 Proportion of inflations outside of the target range for mask leak and tidal volume. RFM; respiratory function monitor
Proportion of inflations outside of the target range for mask leak and tidal volume. RFM; respiratory function monitorFigure 1
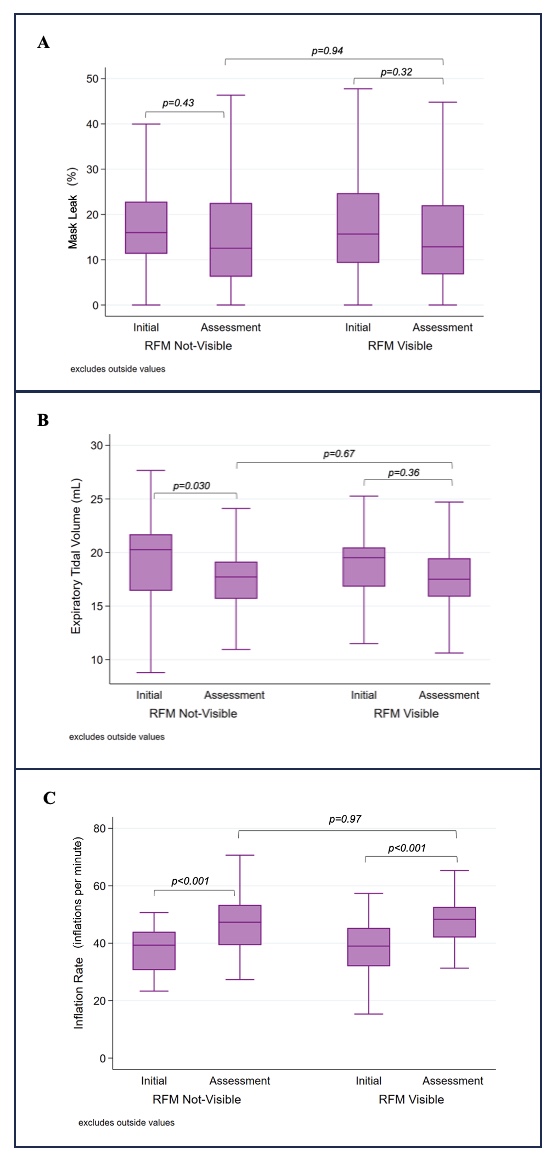 Mask leak (A), expiratory tidal volume (B), inflation rate (C) during 90 seconds of face-mask ventilation for both an initial and assessment session, according to respiratory function monitor (RFM) training group (n=49). The median is represented by the horizontal line in the centre of the box, the interquartile range is shown through the upper and lower boundaries of the box and the whiskers demonstrate the range. A paired t-test and unpaired t-test were performed. P-values are shown on the graphs ( <0.05 statistically significant).
Mask leak (A), expiratory tidal volume (B), inflation rate (C) during 90 seconds of face-mask ventilation for both an initial and assessment session, according to respiratory function monitor (RFM) training group (n=49). The median is represented by the horizontal line in the centre of the box, the interquartile range is shown through the upper and lower boundaries of the box and the whiskers demonstrate the range. A paired t-test and unpaired t-test were performed. P-values are shown on the graphs ( <0.05 statistically significant).
