Neonatal GI Physiology & NEC 3
Session: Neonatal GI Physiology & NEC 3
694 - Towards a Gastric Status Index for Optimizing Enteral Feeding in the Neonatal Intensive Care Unit
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 694.6965
Anoop Rao, Lucile Packard Children's Hospital Stanford, Palo ALto, CA, United States; Rory Geoghegan, Gravitas Medical, Berkeley, CA, United States; Justin Barron, Gravitas Medical, San Mateo, CA, United States; Saheel Sutaria, Gravitas Medical, Inc., Berkeley, CA, United States; Daniel R. Burnett, UCSF, San Francisco, CA, United States; Joanna Jain, Stanford University School of Medicine, Stanford, CA, United States
- AR
Anoop Rao, MD, MS (he/him/his)
Clinical Associate Professor
Lucile Packard Children's Hospital Stanford
Palo ALto, California, United States
Presenting Author(s)
Background: The widely practiced 3-hour feeding cycle in the neonatal intensive care unit has several limitations. Firstly, nutrition is not tailored to the infants’ metabolic requirements thus preventing optimal growth and prolonging length of stay. Secondly, digestive rhythms exhibit inter- and intra-patient variability leading to missed feeding opportunities or conversely overfeeding which may result in the development of feeding intolerance. Finally, it is currently not possible to advance feeding in synchrony with gastric maturity progression. Consequently, there is a great need to develop monitoring technology capable of providing feedback on gastric status thus enabling optimal feeding practices.
Objective: To explore the utility of a novel Gastric Status Index derived from impedance measurements acquired via a sensor integrated feeding tube.
Design/Methods: Gravitas Medical (Berkeley, CA) has developed a feeding tube (FT) with integrated impedance and temperature sensors. This system is capable of assessing gastric status through detection of reflux events and gastric impedance changes induced by filling/emptying of the stomach (Fig. 1). Here, a pilot clinical study was undertaken in which 6 neonates received enteral feeding via the Gravitas FT for 3.3±1.4 days following the standard 3-hour feeding cycle. Sensor data was retrospectively analyzed to identify potential sub-optimal feeding.
Results: Reflux and gastric impedance were successfully recorded throughout the study without any device related adverse events. The Gravitas Gastric Status Index identified missed feeding opportunities (Fig. 2) in all patients indicating potential suboptimal feeding. The per feeding cycle feed volume and reflux duration varied substantially between subjects ranging from 30 to 90ml (Fig 3a) and 0.3 to 2.8 minutes (Fig 3b) respectively. The post-prandial time to return to fasting ranged from 114-190 minutes with large variability observed in 4 subjects highlighting the opportunity to administer feeds as needed rather than strictly adhering to the conventional 3-hour cycle (Fig. 3c). This is further supported by the potential underfeeding noted in subjects B and F where the Gastric Status Index suggests that these subjects were in the fasting state for ~30% of the entire study (Fig. 3d).
Conclusion(s): Sensor integrated feeding tubes can monitor gastric status and have the potential to enable optimized patient-specific feeding in the NICU potentially maximizing growth and development while minimizing the risk of feeding intolerance and unnecessary prolonged length of stay.
Figure 1: The Gravitas feeding tube (a) calculates a Gastric Status Index based on detection of reflux events from impedance sensors in the esophagus (b) and gastric impedance changes measured via sensors in the stomach (c)
.png)
Figure 2: Gastric Status Index identifies missed feeding opportunities – exemplary data from patient E
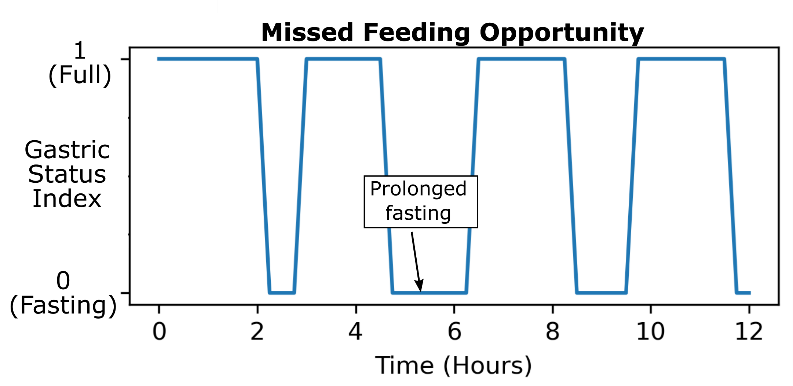
Figure 3: Feed volume (a), reflux duration (b), post-prandial time to return to fasting (c) and time in fasting state (d) throughout study. Note that subjects B and F were potentially underfed as indicated by the combination of lower-than-average feed volumes and prolonged time in the fasting state. [error bars: standard deviation]
.png)

