Neonatal/Infant Resuscitation 3
Session: Neonatal/Infant Resuscitation 3
392 - Perinatal Risk Factors and Delivery Room Resuscitation and Outcomes in Late Preterm and Term Infants
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 392.6445
Nicholas Plachinski, Medical College of Wisconsin, Cedarburg, WI, United States; Erwin T. Cabacungan, Medical College of Wisconsin, Milwaukee, WI, United States; Ke Yan, Medical College of Wisconsin, Milwaukee, WI, United States; Jian Zhang, Medical College of Wisconsin, Milwaukee, WI, United States; Ruby Gupta, Medical College of Wisconsin, Milwaukee, WI, United States

Nicholas Plachinski, DO (he/him/his)
Resident
Medical College of Wisconsin
Cedarburg, Wisconsin, United States
Presenting Author(s)
Background: Resuscitation in the delivery room (DR) is a critical event that can determine the immediate and long-term outcomes for infants. There are identified risk factors for anticipated resuscitation, though not all infants with these risk factors will require intervention. Moreover, there are few infants who need help without risk factors. We hypothesize that identified risk factors can predict intensity of resuscitation and outcomes in these infants.
Objective: To describe the frequency and extent of DR resuscitation and evaluate the association of DR resuscitation with neonatal outcomes in late preterm (LPT) and term (T) infants with maternal and perinatal risk factors.
Design/Methods: This is a retrospective cohort study of LPT, and T infants delivered at ≥34 weeks’ gestational age (GA) at a level 4 delivery hospital who required resuscitation from July 2022 to June 2023. Infants were categorized into 3 groups based on the highest level of respiratory intervention in DR: Grp 1 [Only continuous positive airway pressure (CPAP)]; Grp 2 [positive pressure ventilation (PPV), may have CPAP no endotracheal intubation (ETT)], and Grp 3 [ETT (may have CPAP and/or PPV)]. The Chi-Square or Fisher’s exact test was used for comparison of categorical variables, and the Kruskal-Wallis or Mann-Whitney test was used for continuous variables.
Results: Of 1,592 infants for which the NICU team attended the delivery, 476 (30%) met inclusion criteria (Fig: 1). Most infants were in Grp 2 (51.1%), followed by Grp 1 (43.5%), while only a small number were in Grp 3 (5.5%). Grp 2 had higher incidence of maternal chorioamnionitis (p=0.0047), and with infants showing lower 5-minute Apgar scores (p < 0.0001) and longer NICU stays compared to Grp 1. Grp 3 had similar non-reassuring fetal heart tones as Grp 2 but the highest rate of prenatal congenital anomalies, lowest 5-minute Apgar scores, and longest NICU stays (Tables 1A&B). The CPAP duration remained similar for Grp 1 and those who progressed to requiring PPV and/or ETT (Grps 2&3) [median duration = 6 vs. 5 minutes, p = 0.52], Fig 2A. The maximum FiO2 requirement was lower while on CPAP compared to those on PPV (median FiO2 = 0.4 vs. 0.5, p< 0.0001), Fig 2B.
Conclusion(s): We highlighted the differences in maternal and perinatal factors across the three resuscitation groups. Most infants received CPAP, with similar CPAP durations noted between those stabilized with CPAP and those who later needed PPV and/or ETT. Higher FiO2 needs were observed in infants requiring PPV, indicating the importance of tailored resuscitation to optimize outcomes.
Figure 1
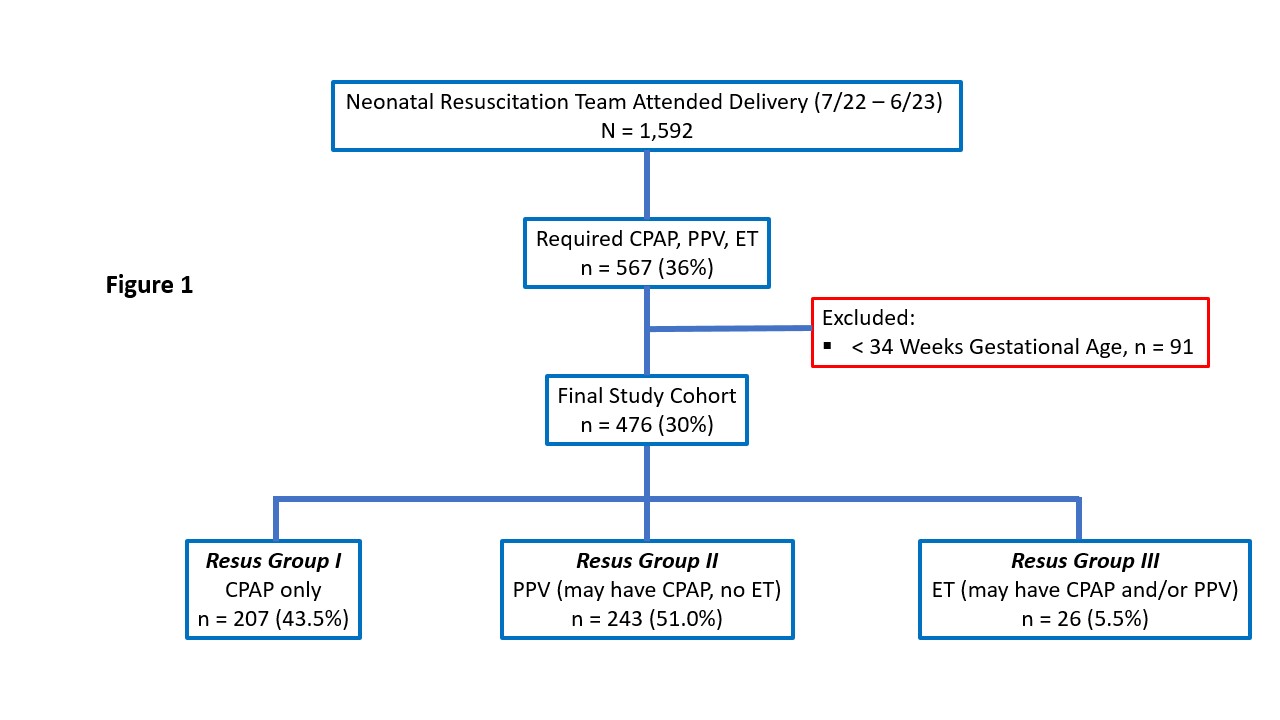 Flow diagram showing the selection process starting with delivery room resuscitation, and to three groups CPAP only, PPV (may have CPAP, no ET), ET (may have CPAP and/or PPV).
Flow diagram showing the selection process starting with delivery room resuscitation, and to three groups CPAP only, PPV (may have CPAP, no ET), ET (may have CPAP and/or PPV).Tables 1A and 1B
.jpg) Table 1A: comparison of maternal demographics and risk factors between the three groups
Table 1A: comparison of maternal demographics and risk factors between the three groupsTable 1B: comparison of antepartum risk factors and infant outcomes between the three groups
Significant p-values bolded in red
Figures 2A and 2B
.jpg) Figure 2A: comparison of CPAP duration between resus group 1 and resus group 2&3.
Figure 2A: comparison of CPAP duration between resus group 1 and resus group 2&3.Figure 2B: comparison of Maximum FiO2 between CPAP vs PPV.

