Neonatal GI Physiology & NEC 4
Session: Neonatal GI Physiology & NEC 4
708 - Clinical Outcomes in Infants with Intestinal Failure: A Ten-Year Single Center Experience in a Surgical NICU
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 708.4546
Gina O'Toole, CHOC Children's Hospital of Orange County, Huntington Beach, CA, United States; Alyson Lawrence, CHOC Children's Hospital of Orange County, Orange, CA, United States; Grant J. Shafer, CHOC Children's Hospital of Orange County, Orange, CA, United States; Adnan Ismail, CHOC Children's Hospital of Orange County/University of California, Irvine, Irvine, CA, United States; Jeffrey Ho, CHOC Children's Hospital of Orange County, Orange, CA, United States; Bassam Younes, UCI, Orange, CA, United States; Mustafa Kabeer, CHOC Children's Hospital of Orange County, Orange, CA, United States; Gholizadeh Maryam, Choc, Orange, CA, United States; Irfan Ahmad, CHOC Children's Hospital of Orange County, Tustin, CA, United States
.jpg)
Gina O'Toole, MPH, RD, CSPCC, CLEC (she/her/hers)
Neonatal Dietitian
CHOC Children's Hospital of Orange County
Huntington Beach, California, United States
Presenting Author(s)
Background: In the neonatal period, the most common cause of intestinal failure (IF) is short bowel syndrome (SBS) resulting from malformations or intestinal surgery. A multi-disciplinary surgical NICU program (SNICU) was developed in 2014. Education and implementation of a comprehensive SBS guideline with standardized approaches to medical management, hepatoprotective total parenteral nutrition (TPN)/IV lipid strategies, and structured enteral feeding practices occurred.
Objective: Our aim was to follow clinical outcomes for infants diagnosed with IF in the NICU during this 10-year period.
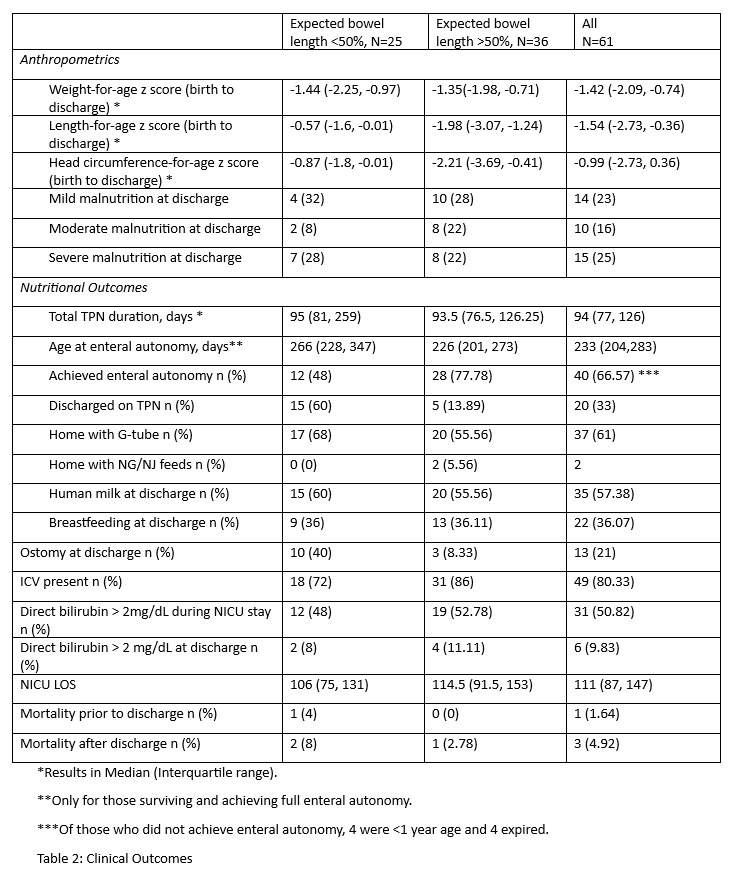
Design/Methods: The SNICU database was queried for infants admitted from January 1, 2014, to December 31, 2023, with IF (defined as TPN requirement for a minimum of 60 days within a 74 consecutive day interval) or discharged home on TPN. IRB approval was obtained. NICU and post discharge medical records were reviewed. Enteral autonomy (EA) was defined as growth adequacy off TPN and on full enteral feeds for a period of 3 months. The cohort was further divided into those who had remaining expected bowel length (EBL) of < 50% or >50% based on published standards.
Results: Out of 385 infants in SNICU with gastrointestinal surgeries, 61 were diagnosed with IF. 33% were female and 80% had an intact ileocecal valve. Among 60 surviving infants at NICU discharge, 33% required TPN and 65% required some tube feeding with gastrostomy or nasogastric/jejunal tubes (NGT/NJT). 51% had cholestasis (direct bilirubin level > 2 mg/dL) during the NICU stay, but only 10% remained cholestatic at discharge. 16% had moderate (z score -1.2 to -2) and 25% severe malnutrition (z score > -2) at discharge. The median length of NICU stay was 111 days with TPN duration of 94 days. More than half went home on human milk and a third were breastfeeding. One infant died prior to discharge and three after discharge. More infants in the < 50% EBL group were discharged with an ostomy (40% vs 8%), on TPN (60% vs 14%), and fewer achieved EA (48% vs 78%).
Conclusion(s): Most infants diagnosed with IF are ultimately able to achieve EA (median of 8 months in this cohort). Few infants had persisting cholestasis at NICU discharge, a testament to the multi-disciplinary care and modern lipid management strategies in these infants. However, the percentage of infants with moderate and severe malnutrition remains high. More research is needed to develop strategies to mitigate malnutrition in this complex population of infants, as non-nutritional complications of inflammation, infection, intestinal dysbiosis and metabolic needs play a key role in nutritional outcomes.
Figure 1
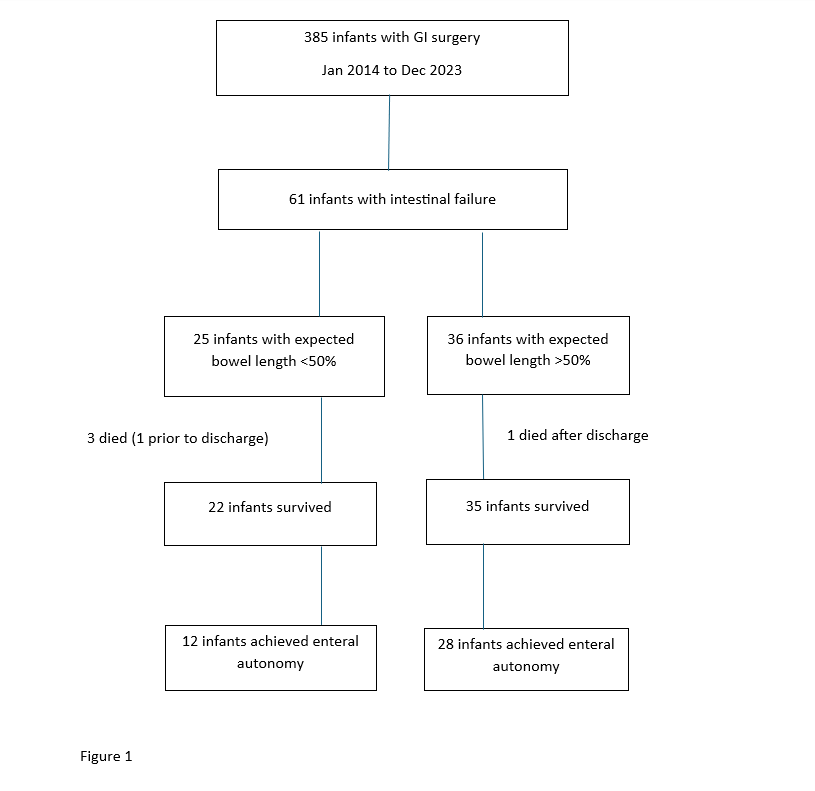
Table 1: Infant Characteristics
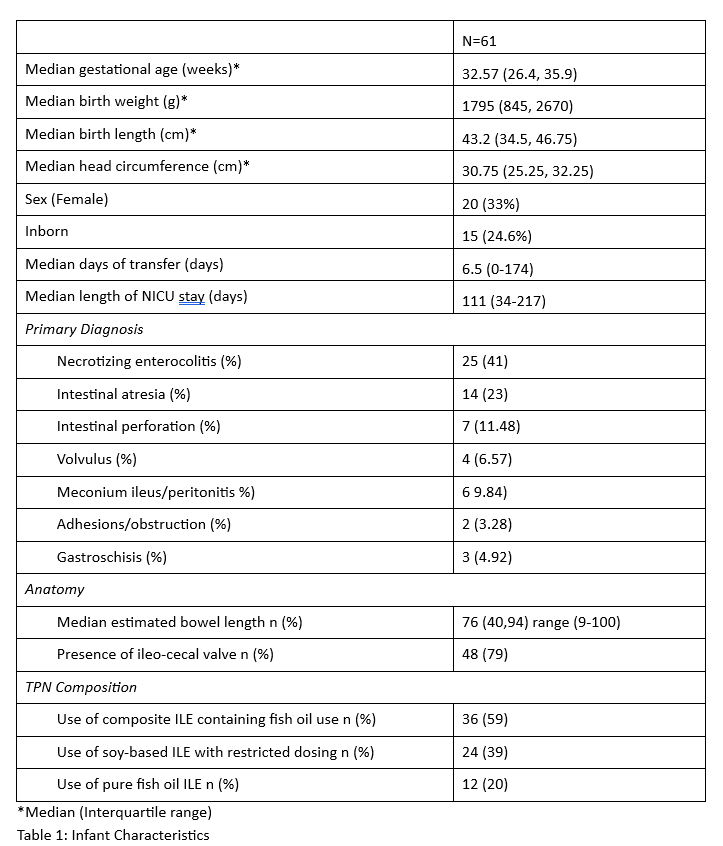
Table 2: Clinical Outcomes