Neonatal/Infant Resuscitation 3
Session: Neonatal/Infant Resuscitation 3
391 - Placental Pathology Differences in Resuscitated Infants: A Comparative Study of Preterm vs. Late Preterm/Term Gestation
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 391.6444

Nicholas Plachinski, DO (he/him/his)
Resident
Medical College of Wisconsin
Cedarburg, Wisconsin, United States
Presenting Author(s)
Background: Placental pathology has been implicated in various adverse neonatal outcomes, including the need for resuscitation at birth. Understanding the relationship between specific placental pathologies and the likelihood of requiring neonatal resuscitation may help inform preventative strategies and tailored resuscitation approaches. We hypothesize that placental pathologies in preterm infants and term infants that need resuscitation will be different.
Objective: To describe and compare the placental pathology findings in infants necessitating delivery room (DR) resuscitation at < 34 weeks vs. ≥34 weeks gestational age (GA)
Design/Methods: A retrospective cohort study was conducted on deliveries at a level 4 delivery hospital between 7/2022 to 6/2023. Neonates who required DR with available placental pathology were categorized by GA groups: Grp 1 [GA < 34 weeks or preterm (PT)] and Grp 2 [GA ≥ 34 weeks or late preterm/term (LPT/T)]. Maternal and antepartum risk factors, infant outcomes, and placental pathology reports were reviewed based on the Amsterdam Placental Pathology Consensus. In addition, we assessed placental weight percentiles and noted conditions such as placenta accreta and meconium-laden macrophages. Differences between the groups were evaluated using Chi-square, Fisher’s exact, Kruskal Wallis, or Student’s T-tests.
Results: Out of 227 available placental pathology, 184 were included (Figure:1). Grp 2 had more White race, partnered status, higher BMI, chorioamnionitis, GBS positivity, meconium-stained fluid, Apgar scores, and birth weight. Grp 1 had more antibiotic/steroid use, prolonged membrane rupture, and emergency c-sections (Tables 1A&B). Grp 2 had heavier placental weights, larger placentas, and more meconium-laden macrophages. Inflammatory lesions were higher in Grp 1, while maternal and fetal vascular malperfusions (FVM) and normal placentas were more common in Grp 2.
Conclusion(s): Placental pathologies show distinct patterns in PT and LPT/T infants requiring DR resuscitation. Meconium-laden macrophages and FVM appear to be significant factors in resuscitation needs in LPT/T, while inflammatory lesions are more influential in PT deliveries. These findings suggest the potential for targeted prenatal interventions based on placental pathology and gestational age.
Figure 1. Flow diagram
.jpg) Flow diagram showing the selection process starting with initial resuscitation to those with placental specimens, and to two groups [ < 34 weeks (PT) vs. ≥ 34 weeks (LPT/T)]
Flow diagram showing the selection process starting with initial resuscitation to those with placental specimens, and to two groups [ < 34 weeks (PT) vs. ≥ 34 weeks (LPT/T)]Table 1A and 1B
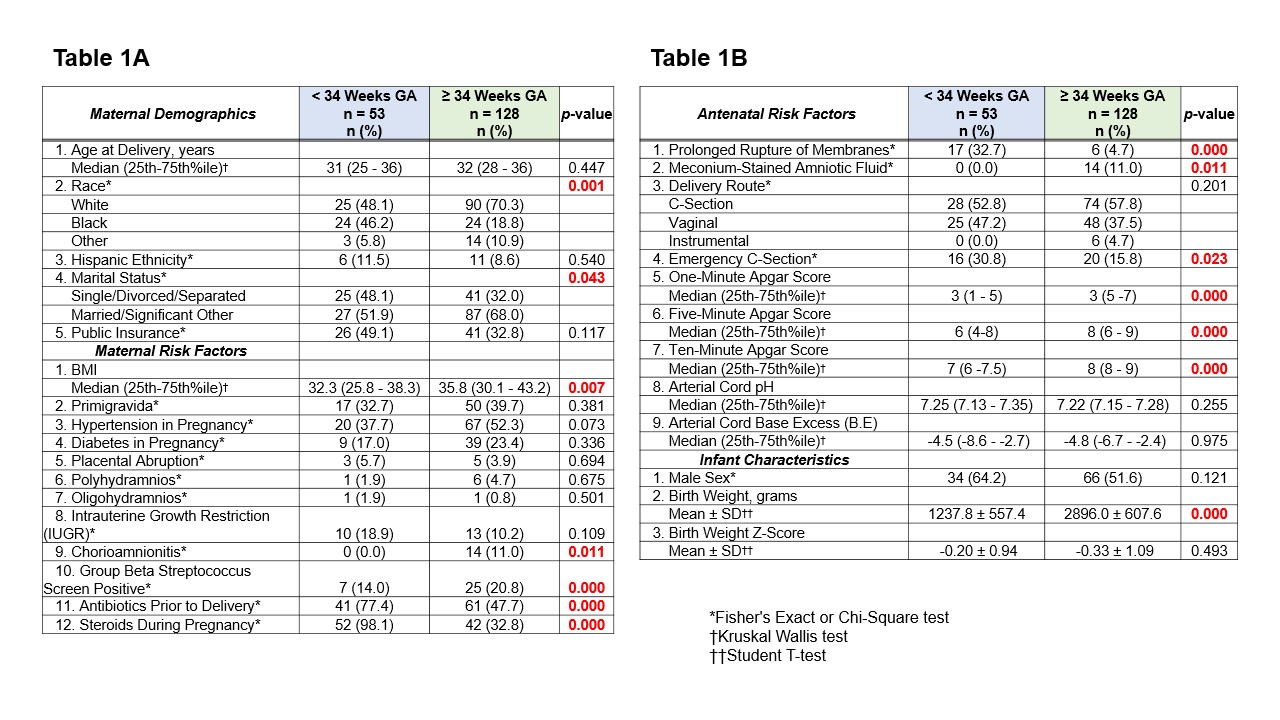 Table 1A . Comparison of maternal demographics and risk factors between the two groups [ < 34 weeks (PT) vs. ≥ 34 weeks (LPT/T)].
Table 1A . Comparison of maternal demographics and risk factors between the two groups [ < 34 weeks (PT) vs. ≥ 34 weeks (LPT/T)]. Table 1B. Comparison of antenatal risk factors and infant characteristics between the two groups [ < 34 weeks (PT) vs. ≥ 34 weeks (LPT/T)].
Significant p-values are highlighted in bold red.
Table 2
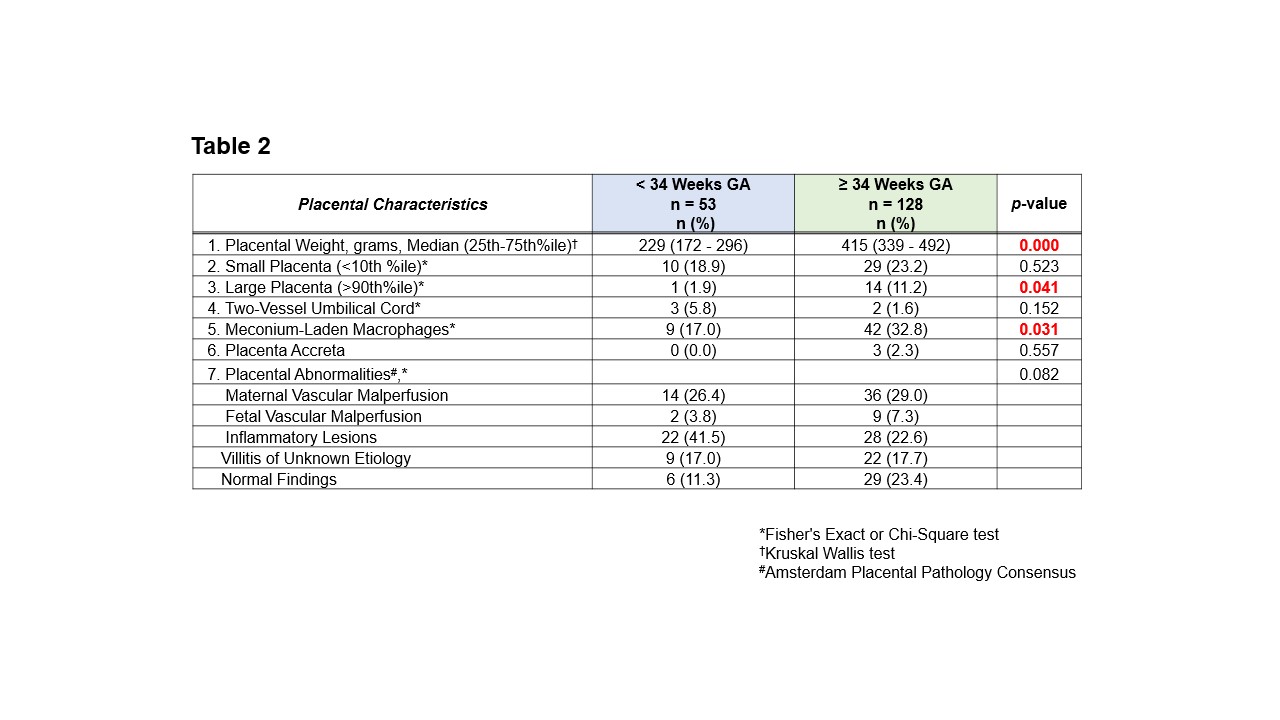 Comparison of placental pathology differences between the two groups [ < 34 weeks (PT) vs. ≥ 34 weeks (LPT/T)], with placental abnormalities categorized according to the Amsterdam Placental Pathology Consensus. Significant p-values are highlighted in bold red.
Comparison of placental pathology differences between the two groups [ < 34 weeks (PT) vs. ≥ 34 weeks (LPT/T)], with placental abnormalities categorized according to the Amsterdam Placental Pathology Consensus. Significant p-values are highlighted in bold red.
