Neonatal Hematology & Bilirubin Metabolism 2
Session: Neonatal Hematology & Bilirubin Metabolism 2
678 - Platelet count trends in extremely premature newborns in the first week of life
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 678.6356
Edson Ruiz, Le Bonheur Children's Hospital, Memphis, TN, United States; Ajay J. Talati, University of Tennessee Health Science Center, Memphis, TN, United States

Edson Ruiz, MD
Assistant professor
Le Bonheur Children's Hospital
Memphis, Tennessee, United States
Presenting Author(s)
Background: Platelet abnormalities are a common problem in the NICU. Due to this common scenario, studies have tried determining platelet indices in newborns without many of them focusing on the most affected subpopulation of newborns, the extremely preterm
Objective: We aim to establish platelet count ranges within the first week of life for newborns < 27 weeks of gestation and assess the correlation of platelet count with clinical outcomes.
Design/Methods: A retrospective study was conducted at Regional One Hospital in Memphis, TN, after IRB approval. We included babies born at < 27 wk
gestation who received ICU care for at least 24 h. We excluded newborns who received comfort care or died within the first 24 hours of life or those with missing records of platelet counts during the first week of life. 243 patients met the inclusion criteria, 48 patients were excluded. Data from 191 patients included demographic information and clinical variables as shown in table 1.
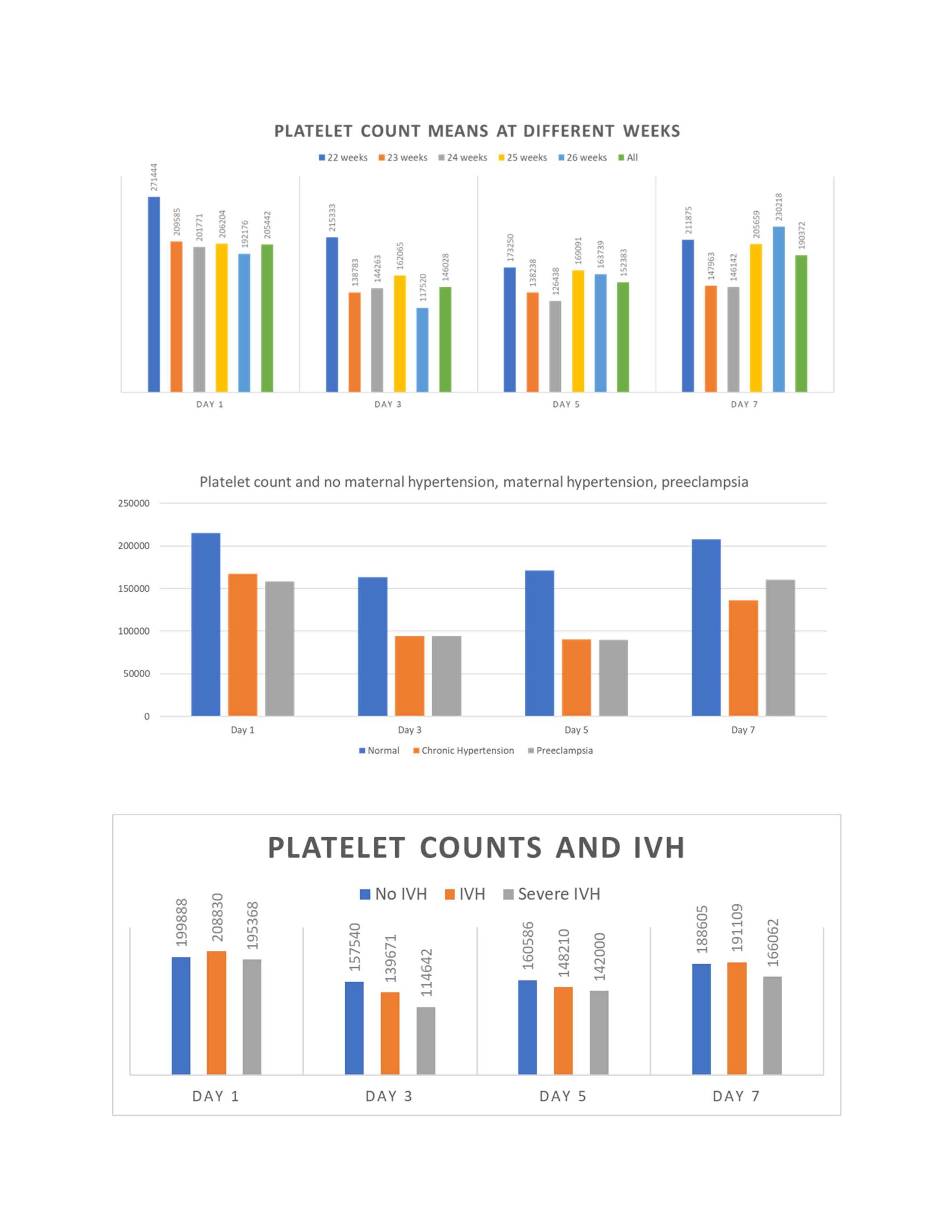
Results: A total of 191 neonates were included in the study, out of which 90 were female. Of the 191 extremely preterm neonates, 51 (26.7%) died before discharge. As shown in Table 1, the mean gestational age for the entire cohort was 24.5 wk, and the mean birth weight was 690 grams. Table 1 also shows the demographic data of the cohorts for each week of EGA at birth. The mean platelet counts for the entire cohort on day one of life was 205442 ±77824/μL (median 202500), day three of life mean 146028 ± 87332 /μL (median 126000); day five of life mean 152383 ±97419/μL (median 120000), day seven mean 190372 ± 106373 /μL (median 177000). Newborns from mothers with chronic hypertension or any preeclampsia had lower initial platelet counts, with an increase in their numbers by day seven (Table 3). Platelet counts on those newborns with severe IVH trended lower on days three and five as compared with newborns without IVH in newborns at 22-24 weeks; however, they did not reach statistical significance (Table 3).
Conclusion(s): Our data support the currently acceptable normal values (as defined in late preterm and term infants) in this extremely preterm population. Furthermore, maternal and placental conditions like hypertension/preeclampsia and intra-uterine growth restriction significantly decreased platelet counts in preterm neonates, which seemed to recover by the end of the first week. However, lower platelet counts at birth were not associated with severe IVH and pulmonary hemorrhage. This supports the idea of not transfusing asymptomatic patients to keep platelet counts above a specific number. Further RCTs will clarify this clinical dilemma
Table 1
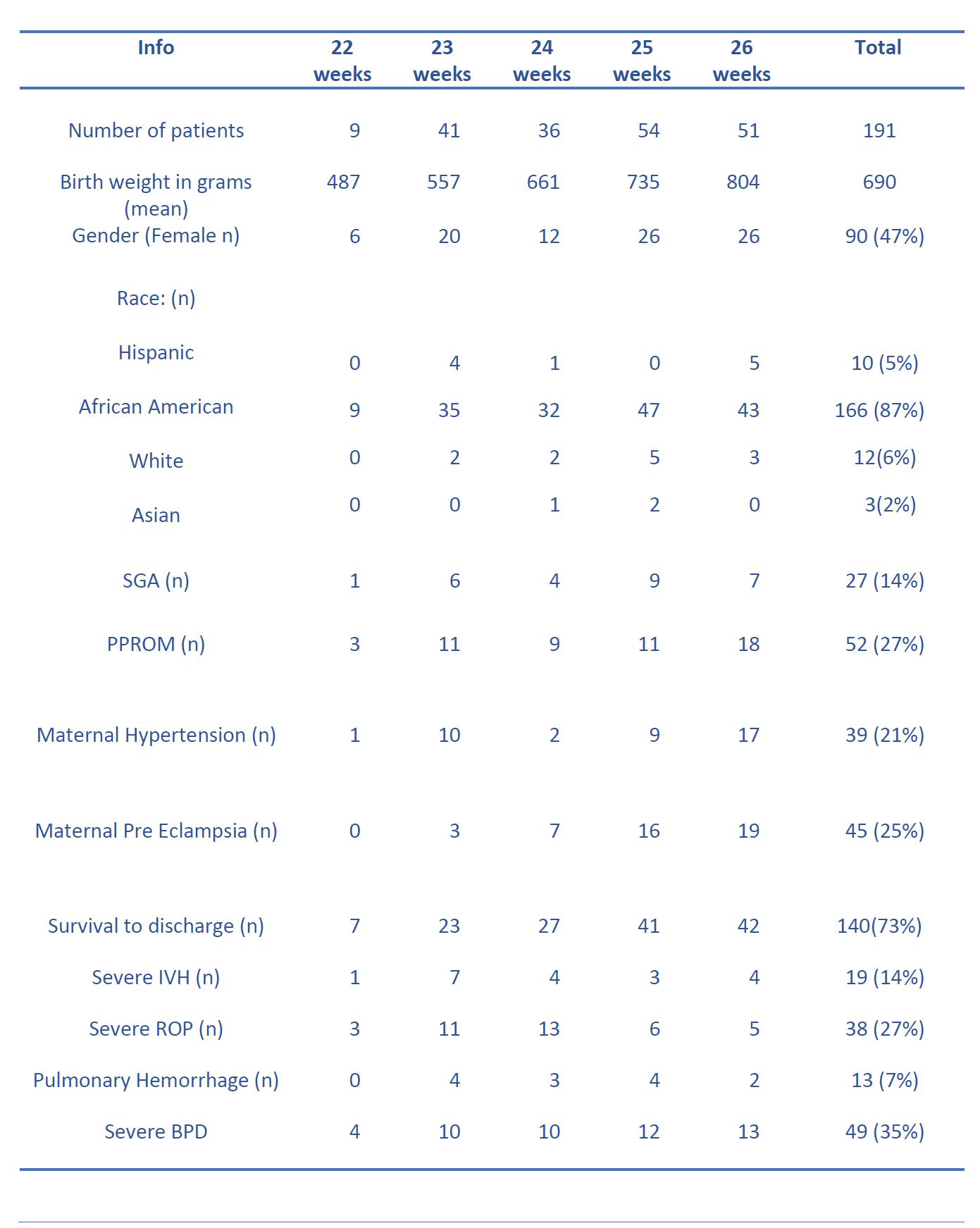
Table 2-3 (statistical analysis)
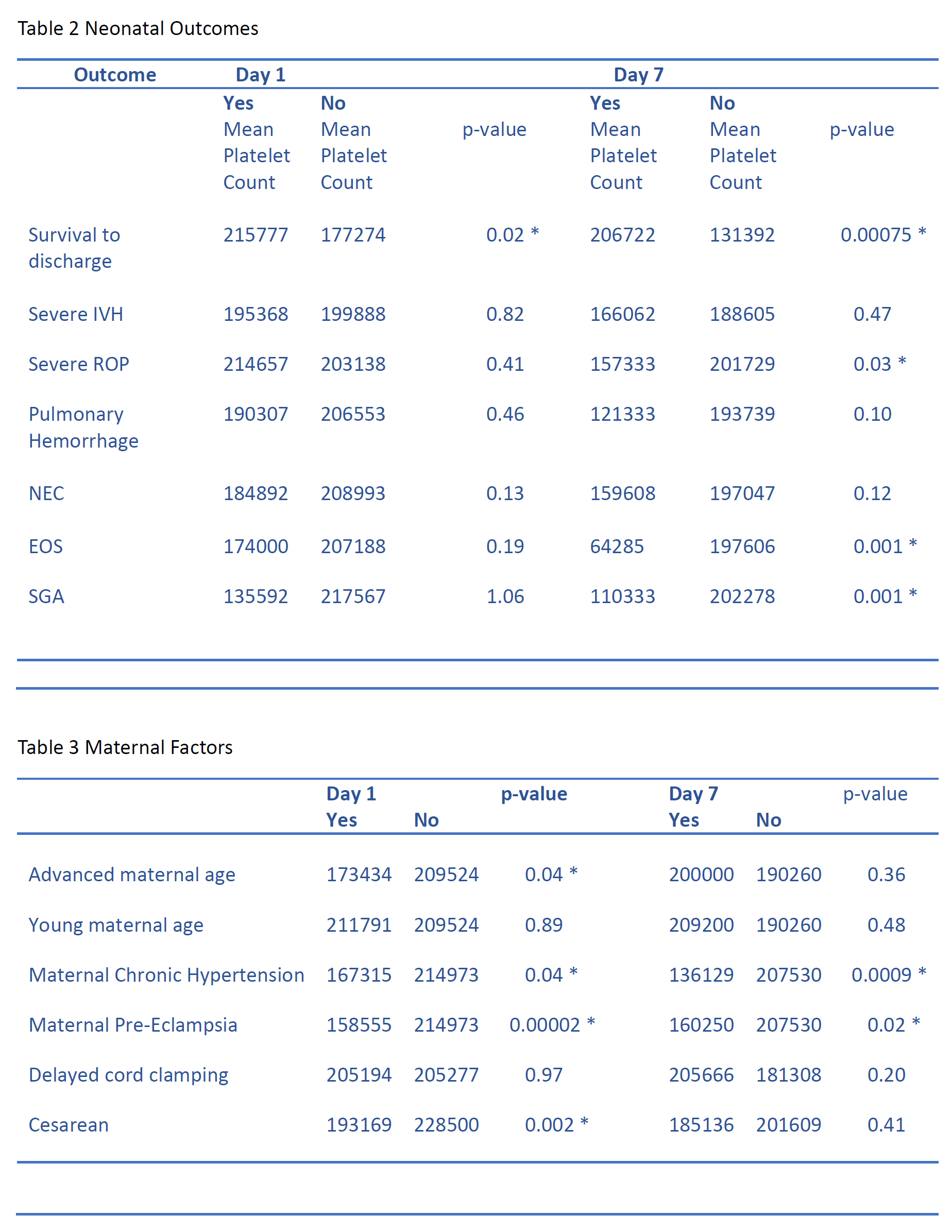
Table 3