Neonatal General 10: Family Centered Care and Social Determinants of Health
Session: Neonatal General 10: Family Centered Care and Social Determinants of Health
234 - Racial and ethnic disparities in postnatal growth for infants born between 23 and 29 weeks of gestation
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 234.6169
Crystal Hsueh, University of California, Los Angeles, Los Angeles, CA, United States; Hung-Wen Yeh, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Reese H. Clark, Duke University School of Medicine, Marietta, SC, United States; Ashwini Lakshmanan, Kaiser Permanente Bernard J. Tyson School of Medicine, Pasadena, CA, United States; Fu-Sheng Chou, Kaiser Permanente Bernard J. Tyson School of Medicine, Riverside, CA, United States
- CH
Crystal Hsueh, Bachelor of Science (she/her/hers)
Student
University of California, Los Angeles
Los Angeles, California, United States
Presenting Author(s)
Background: Disparities in birth size, growth rates, and the likelihood of postnatal growth faltering among preterm infants exist, but a detailed understanding of disparities across different growth phases is lacking.
Objective: This study aims to evaluate racial/ethnic disparities in (1) Birth weight (BW), (2) time to BW regain, and (3) mean growth velocity (GV) between DOL 10 and 34 weeks PMA.
Design/Methods: We conducted a retrospective cohort study using data from the Pediatrix Clinical Data Warehouse (CDW), categorizing race/ethnicity into five groups: White, Black, Hispanic, Asian, and Other. Infants born between 23 and 29 weeks’ gestation were included. Race/ethnicity-specific intrauterine growth charts were created for BW z-score referencing: For (1) BW comparison, BW was referenced to White. For (2) time-to-BW-regain and (3) mean GV analyses, BW was referenced to respective race/ethnicity (as a covariate) or White (as an additional confounder). The selection criteria are listed in Fig 1A. Antenatal confounders listed in Fig 1B were balanced using inverse propensity score weighting (Fig 1C). Mixed-effect models adjusting for covariates and accounting for facility-level differences were developed.
Results: We included 76,145 infants. Confounder variables were balanced to create a weighted population of 374,832 infants (Fig 1B vs 1C). For disparities in BW z-scores, compared to White (0.08 [0.06, 0.10]), Black (-0.08 [-0.10, -0.06]) and Asian (0.01 [-0.06, 0.08]) infants had significantly lower z-scores, while Hispanic infants (0.12 [0.09, 0.16]) had significantly higher z-scores (Fig 2A). For time to BW regain, Black (9.0 [8.9,9.2] days) took significantly less time to regain BW compared to White (9.9 [9.7, 10.0] days), while Hispanics (10.0 [9.8, 10.3] days) took significantly longer (Fig 2B). Faster BW regain in Black is independent of BW, but slower BW regain in Hispanics is due to higher BW z-scores (Fig 2B vs 3A). Finally, compared to White (17.3 [17.2, 17.5] g/kg/day), Hispanic infants (16.9 [16.6, 17.1] g/kg/day) had significantly lower mean GV between DOL10 and 34 weeks PMA. No significant differences were observed in other racial/ethnic groups (Fig 2C). GV disparity was independent of BW z-scores (Fig 2C vs 3B).
Conclusion(s): Racial/ethnic disparities exist in the postnatal growth of preterm infants, with Black infants being born the smallest but showing catch-up growth when compared to White, and Hispanic infants being born the largest but experiencing slower postnatal growth. The findings from this study highlight opportunities for targeted interventions to reduce disparities in neonatal care.
Figure 1. Establishing an infant cohort using selection criteria to develop a weighted population for analysis.
.jpg) (A) A diagram showing the inclusion and exclusion criteria for each aim, along with the number of infants before and after applying inverse propensity score weighting. Confounders balanced include maternal age, gestational age, sex, maternal obesity, hypertensive disorders of pregnancy, fetal growth restriction, maternal smoking during pregnancy, placental abruption, gestational diabetes, chorioamnionitis, and congenital anomalies. Propensity scores were derived using generalized boosted regression modeling to estimate the population average treatment effect. (B) Maternal and neonatal characteristics of the unweighted cohort. (C) Maternal and neonatal characteristics of the weighted population.
(A) A diagram showing the inclusion and exclusion criteria for each aim, along with the number of infants before and after applying inverse propensity score weighting. Confounders balanced include maternal age, gestational age, sex, maternal obesity, hypertensive disorders of pregnancy, fetal growth restriction, maternal smoking during pregnancy, placental abruption, gestational diabetes, chorioamnionitis, and congenital anomalies. Propensity scores were derived using generalized boosted regression modeling to estimate the population average treatment effect. (B) Maternal and neonatal characteristics of the unweighted cohort. (C) Maternal and neonatal characteristics of the weighted population.Figure 2. Regression analysis estimating racial and ethnic disparities in birth weight z-scores, time-to-birth-weight- regain, and mean growth velocity during the accelerated growth phase.
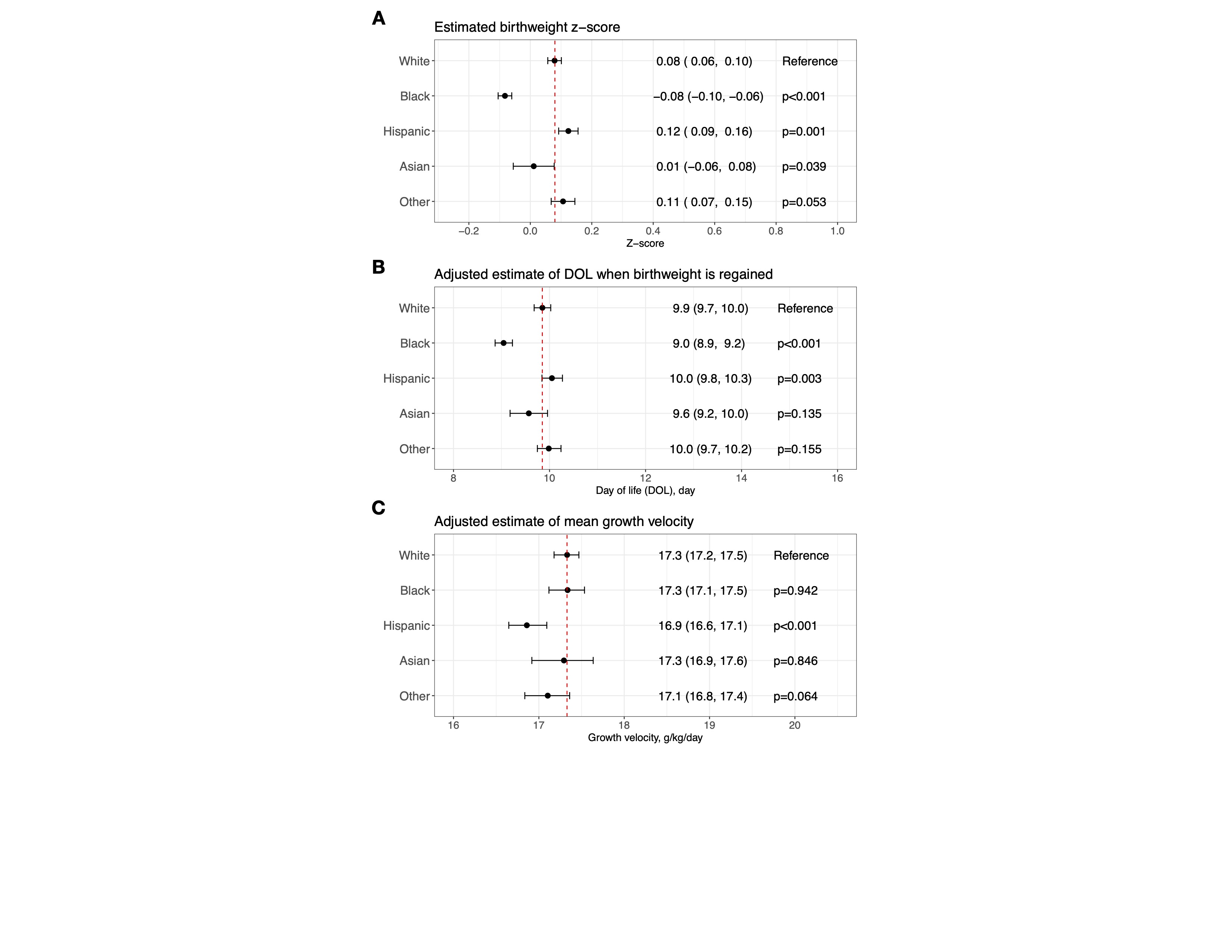 (A) A mixed-effects model was developed to assess racial and ethnic disparities in birth weight z-scores based on the entire weighted population shown in Figure 1C. The birth weight z-scores were calculated using intrauterine growth charts developed for White infants as part of this study. White was used as the reference. (B) A mixed-effects model was developed to assess racial and ethnic disparities in time-to-birth-weight-regain, based on a weighted subpopulation of infants who regained their birth weight by day of life (DOL) 27 (Figure 1A). The model was adjusted for APGAR scores at 1 and 5 minutes and birth weight z-scores, calculated using race/ethnicity-specific intrauterine growth charts developed for this study (for adjusting within each racial/ethnic group). Time-to-birth-weight-regain for White was used as the reference. (C) A mixed-effects model was developed to assess racial and ethnic disparities in mean growth velocity, using a weighted subpopulation of infants with a weight nadir by DOL10 and birth weight regained by DOL27 (Figure 1A). Mean growth velocity was calculated based on daily weight measurements from DOL10 to the last recorded weight between 33-34 weeks postmenstrual age. The model was adjusted for several covariates: APGAR scores at 1 and 5 minutes, birth weight z-scores (calculated using race/ethnicity-specific intrauterine growth charts developed for this study), grade 2/3 bronchopulmonary dysplasia, stage 2-5 retinopathy of prematurity, retinopathy of prematurity receiving treatment, patent ductus arteriosus receiving treatment, medical or surgical necrotizing enterocolitis, intestinal perforation, grade 3/4 intraventricular hemorrhage, total days on antibiotics after DOL3, and postnatal corticosteroid use. Mean growth velocity for White was used as the reference.
(A) A mixed-effects model was developed to assess racial and ethnic disparities in birth weight z-scores based on the entire weighted population shown in Figure 1C. The birth weight z-scores were calculated using intrauterine growth charts developed for White infants as part of this study. White was used as the reference. (B) A mixed-effects model was developed to assess racial and ethnic disparities in time-to-birth-weight-regain, based on a weighted subpopulation of infants who regained their birth weight by day of life (DOL) 27 (Figure 1A). The model was adjusted for APGAR scores at 1 and 5 minutes and birth weight z-scores, calculated using race/ethnicity-specific intrauterine growth charts developed for this study (for adjusting within each racial/ethnic group). Time-to-birth-weight-regain for White was used as the reference. (C) A mixed-effects model was developed to assess racial and ethnic disparities in mean growth velocity, using a weighted subpopulation of infants with a weight nadir by DOL10 and birth weight regained by DOL27 (Figure 1A). Mean growth velocity was calculated based on daily weight measurements from DOL10 to the last recorded weight between 33-34 weeks postmenstrual age. The model was adjusted for several covariates: APGAR scores at 1 and 5 minutes, birth weight z-scores (calculated using race/ethnicity-specific intrauterine growth charts developed for this study), grade 2/3 bronchopulmonary dysplasia, stage 2-5 retinopathy of prematurity, retinopathy of prematurity receiving treatment, patent ductus arteriosus receiving treatment, medical or surgical necrotizing enterocolitis, intestinal perforation, grade 3/4 intraventricular hemorrhage, total days on antibiotics after DOL3, and postnatal corticosteroid use. Mean growth velocity for White was used as the reference.Figure 3. Mechanistic interrogation of the role of birth size (weight z-scores) in racial and ethnic disparities related to time-to-birth-weight-regain and mean growth velocity during the accelerated growth phase.
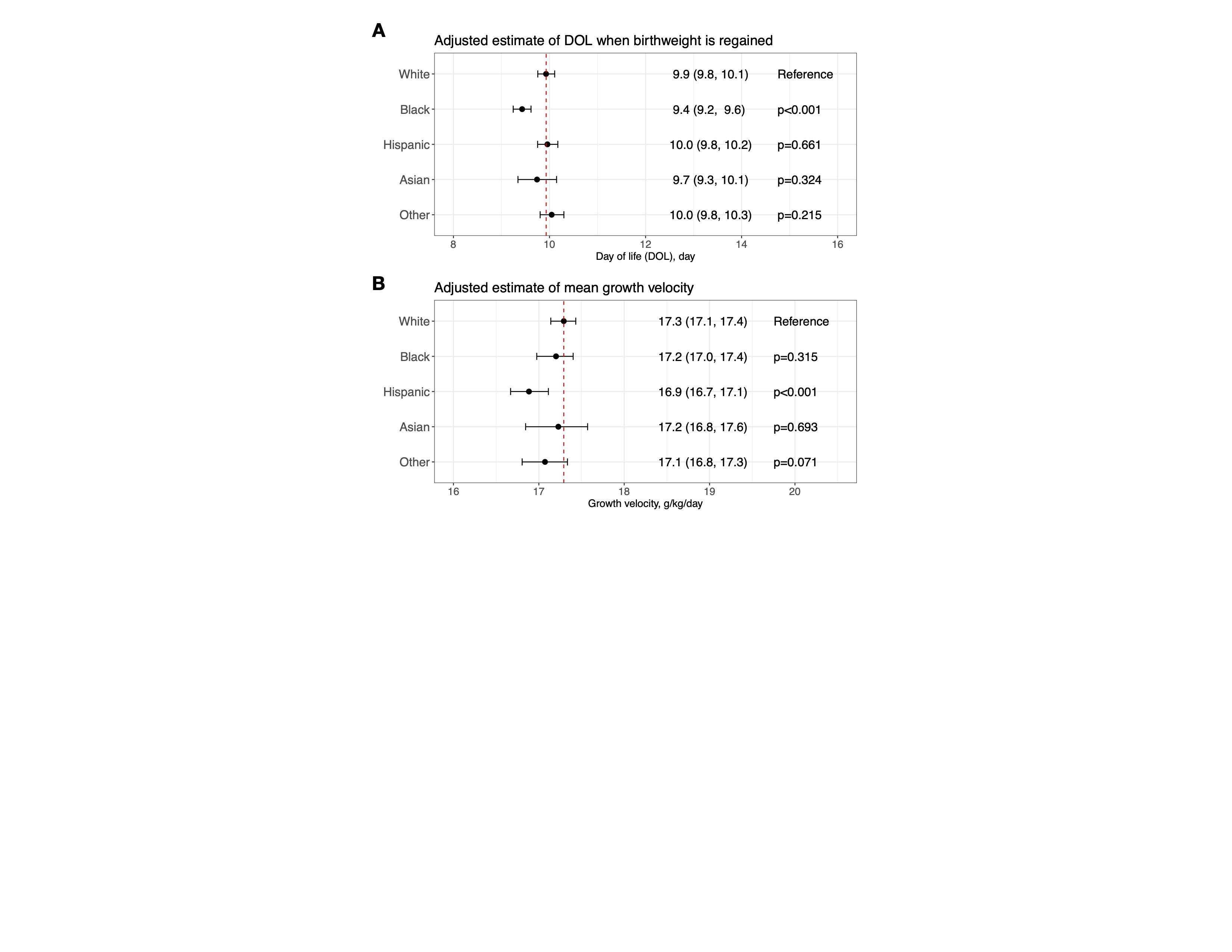 (A) Re-analysis of Figure 2B, using birth weight z-scores calculated from intrauterine growth charts for White infants as a confounder. (B) Re-analysis of Figure 2C, using birth weight z-scores calculated from intrauterine growth charts for White infants as a confounder. The rationale for using intrauterine growth charts for White to calculate birth weight z-scores for adjusting in these re-analyses is to treat birth weight z-scores as a confounder.
(A) Re-analysis of Figure 2B, using birth weight z-scores calculated from intrauterine growth charts for White infants as a confounder. (B) Re-analysis of Figure 2C, using birth weight z-scores calculated from intrauterine growth charts for White infants as a confounder. The rationale for using intrauterine growth charts for White to calculate birth weight z-scores for adjusting in these re-analyses is to treat birth weight z-scores as a confounder.Figure 1. Establishing an infant cohort using selection criteria to develop a weighted population for analysis.
.jpg) (A) A diagram showing the inclusion and exclusion criteria for each aim, along with the number of infants before and after applying inverse propensity score weighting. Confounders balanced include maternal age, gestational age, sex, maternal obesity, hypertensive disorders of pregnancy, fetal growth restriction, maternal smoking during pregnancy, placental abruption, gestational diabetes, chorioamnionitis, and congenital anomalies. Propensity scores were derived using generalized boosted regression modeling to estimate the population average treatment effect. (B) Maternal and neonatal characteristics of the unweighted cohort. (C) Maternal and neonatal characteristics of the weighted population.
(A) A diagram showing the inclusion and exclusion criteria for each aim, along with the number of infants before and after applying inverse propensity score weighting. Confounders balanced include maternal age, gestational age, sex, maternal obesity, hypertensive disorders of pregnancy, fetal growth restriction, maternal smoking during pregnancy, placental abruption, gestational diabetes, chorioamnionitis, and congenital anomalies. Propensity scores were derived using generalized boosted regression modeling to estimate the population average treatment effect. (B) Maternal and neonatal characteristics of the unweighted cohort. (C) Maternal and neonatal characteristics of the weighted population.Figure 2. Regression analysis estimating racial and ethnic disparities in birth weight z-scores, time-to-birth-weight- regain, and mean growth velocity during the accelerated growth phase.
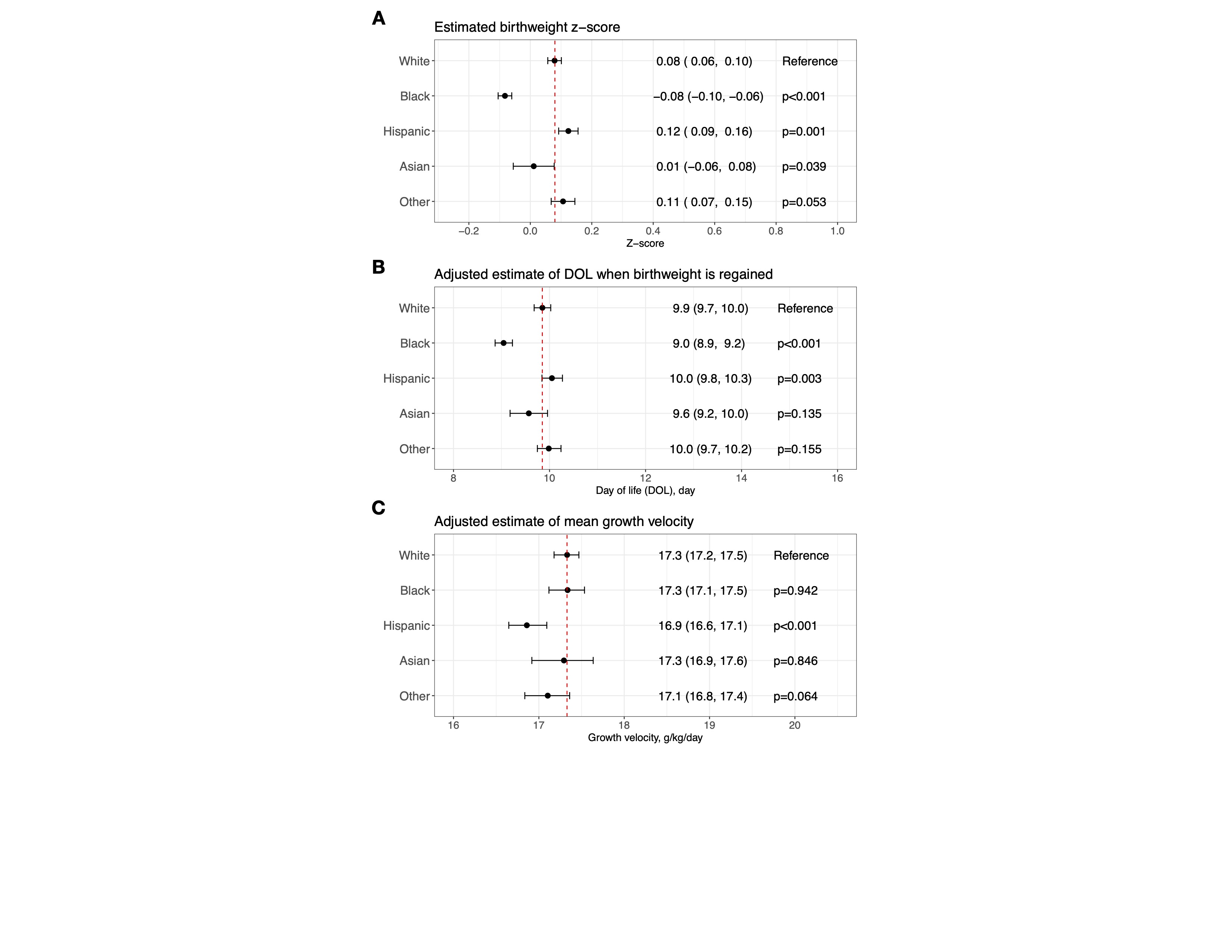 (A) A mixed-effects model was developed to assess racial and ethnic disparities in birth weight z-scores based on the entire weighted population shown in Figure 1C. The birth weight z-scores were calculated using intrauterine growth charts developed for White infants as part of this study. White was used as the reference. (B) A mixed-effects model was developed to assess racial and ethnic disparities in time-to-birth-weight-regain, based on a weighted subpopulation of infants who regained their birth weight by day of life (DOL) 27 (Figure 1A). The model was adjusted for APGAR scores at 1 and 5 minutes and birth weight z-scores, calculated using race/ethnicity-specific intrauterine growth charts developed for this study (for adjusting within each racial/ethnic group). Time-to-birth-weight-regain for White was used as the reference. (C) A mixed-effects model was developed to assess racial and ethnic disparities in mean growth velocity, using a weighted subpopulation of infants with a weight nadir by DOL10 and birth weight regained by DOL27 (Figure 1A). Mean growth velocity was calculated based on daily weight measurements from DOL10 to the last recorded weight between 33-34 weeks postmenstrual age. The model was adjusted for several covariates: APGAR scores at 1 and 5 minutes, birth weight z-scores (calculated using race/ethnicity-specific intrauterine growth charts developed for this study), grade 2/3 bronchopulmonary dysplasia, stage 2-5 retinopathy of prematurity, retinopathy of prematurity receiving treatment, patent ductus arteriosus receiving treatment, medical or surgical necrotizing enterocolitis, intestinal perforation, grade 3/4 intraventricular hemorrhage, total days on antibiotics after DOL3, and postnatal corticosteroid use. Mean growth velocity for White was used as the reference.
(A) A mixed-effects model was developed to assess racial and ethnic disparities in birth weight z-scores based on the entire weighted population shown in Figure 1C. The birth weight z-scores were calculated using intrauterine growth charts developed for White infants as part of this study. White was used as the reference. (B) A mixed-effects model was developed to assess racial and ethnic disparities in time-to-birth-weight-regain, based on a weighted subpopulation of infants who regained their birth weight by day of life (DOL) 27 (Figure 1A). The model was adjusted for APGAR scores at 1 and 5 minutes and birth weight z-scores, calculated using race/ethnicity-specific intrauterine growth charts developed for this study (for adjusting within each racial/ethnic group). Time-to-birth-weight-regain for White was used as the reference. (C) A mixed-effects model was developed to assess racial and ethnic disparities in mean growth velocity, using a weighted subpopulation of infants with a weight nadir by DOL10 and birth weight regained by DOL27 (Figure 1A). Mean growth velocity was calculated based on daily weight measurements from DOL10 to the last recorded weight between 33-34 weeks postmenstrual age. The model was adjusted for several covariates: APGAR scores at 1 and 5 minutes, birth weight z-scores (calculated using race/ethnicity-specific intrauterine growth charts developed for this study), grade 2/3 bronchopulmonary dysplasia, stage 2-5 retinopathy of prematurity, retinopathy of prematurity receiving treatment, patent ductus arteriosus receiving treatment, medical or surgical necrotizing enterocolitis, intestinal perforation, grade 3/4 intraventricular hemorrhage, total days on antibiotics after DOL3, and postnatal corticosteroid use. Mean growth velocity for White was used as the reference.Figure 3. Mechanistic interrogation of the role of birth size (weight z-scores) in racial and ethnic disparities related to time-to-birth-weight-regain and mean growth velocity during the accelerated growth phase.
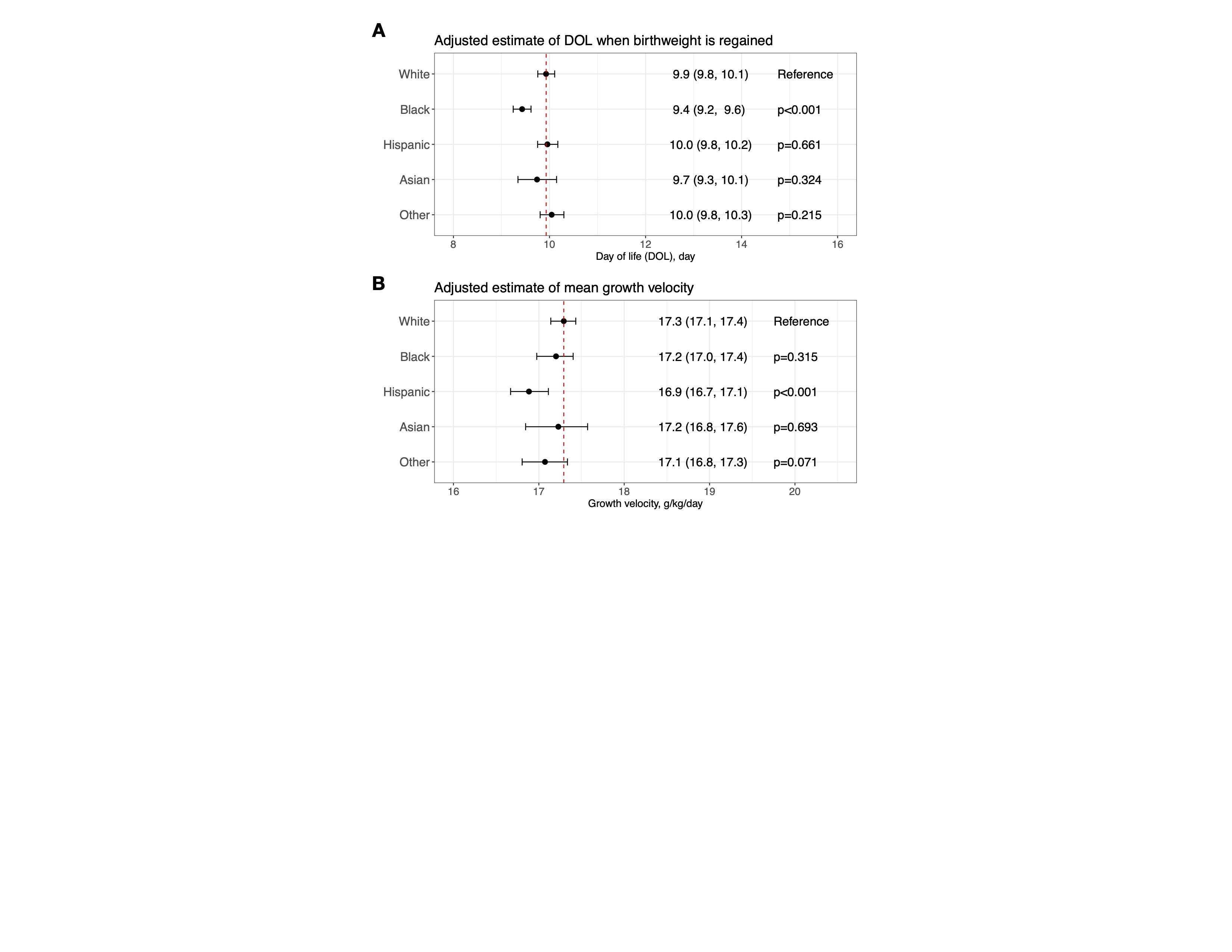 (A) Re-analysis of Figure 2B, using birth weight z-scores calculated from intrauterine growth charts for White infants as a confounder. (B) Re-analysis of Figure 2C, using birth weight z-scores calculated from intrauterine growth charts for White infants as a confounder. The rationale for using intrauterine growth charts for White to calculate birth weight z-scores for adjusting in these re-analyses is to treat birth weight z-scores as a confounder.
(A) Re-analysis of Figure 2B, using birth weight z-scores calculated from intrauterine growth charts for White infants as a confounder. (B) Re-analysis of Figure 2C, using birth weight z-scores calculated from intrauterine growth charts for White infants as a confounder. The rationale for using intrauterine growth charts for White to calculate birth weight z-scores for adjusting in these re-analyses is to treat birth weight z-scores as a confounder.
