Neonatal General 11
Session: Neonatal General 11
418 - Transport Characteristics for Preterm Versus Term Infants with Congenital Diaphragmatic Hernia
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 418.6573
Katrin Lichtsinn, Seattle Children's, Seattle, WA, United States; Daniel A. Enquobahrie, University of Washington, Seattle, WA, United States; John Feltner, University of Washington School of Medicine, Seattle, WA, United States; Megan Gray, University of Washington School of Medicine, Seattle, WA, United States; Rachel A.. Umoren, University of Washington, Seattle, WA, United States; Zeenia Billimoria, University of Washington School of Medicine, Seattle, WA, United States
- KL
Katrin Lichtsinn, MD, MS (she/her/hers)
Assistant Professor of Pediatrics
Seattle Children's
Seattle, Washington, United States
Presenting Author(s)
Background: Newborns with severe congenital anomalies have a significant risk of clinical deterioration during neonatal transport. Premature infants with congenital diaphragmatic hernia (CDH) may be at higher risk for transport decompensation. Predictors of CDH severity, including observed-to-expected total fetal lung volume (O/E TFLV) and lung-to-head ratio (O/E LHR) can inform patient management including transfer to a regional Level IV neonatal intensive care unit.
Objective: Assess transport characteristics, including transport duration and vital sign abnormalities, for preterm (born < 37 completed weeks of gestation) vs term infants with CDH.
Design/Methods: Retrospective study of infants with prenatally diagnosed CDH transported by a pediatric critical care transport team from referring to receiving facility from 2020-2024. Chart-based demographic and clinical data, including transport vital signs and transport times were abstracted. Infants were categorized based on CDH severity using O/E TFLV (based on prenatal MRI) or by O/E LHR (using ultrasound): mild (≥35%), moderate (25-34%), and severe ( < 25%). Vital sign abnormalities were defined using clinical standards. Outcomes of interest included the number of infants with at least one vital sign abnormality and the timing of transport milestones. Kruskal-Wallis or Fisher’s exact tests were used to compare clinical characteristics and vital sign abnormalities across preterm and term infants.
Results: 51 infants were included; 40 (78%) term and 11 (22%) preterm. There was no difference in predicted CDH severity between groups (Table 1). Significantly more preterm infants had cardiac (45% vs 13%, p=0.03) and other congenital anomalies (82% vs 43%, p=0.04) compared to term infants. There was no difference in extracorporeal membrane oxygenation (ECMO) use, survival to discharge, or hospital days between the groups (Table 1). More preterm infants received vasopressors on transport compared to term infants (36% vs 3%, p=0.006) and had a shorter duration from birth to transfer of care at the receiving facility (66min [57-183] vs 156min [80-216], p=0.04). There were no statistically significant differences in other transport times (Table 2) or percent of infants experiencing at least one vital sign abnormality (Table 3).
Conclusion(s): Besides congenital anomalies, there were few other significant differences in clinical characteristics (including vital sign abnormality) between CDH infants who were preterm vs term. Preterm infants had a faster time from birth to transfer and received more vasopressor support, which may have implications for transport team preparedness.
Table 1. Demographics and hospital course variables for infants with CDH stratified by gestational age.
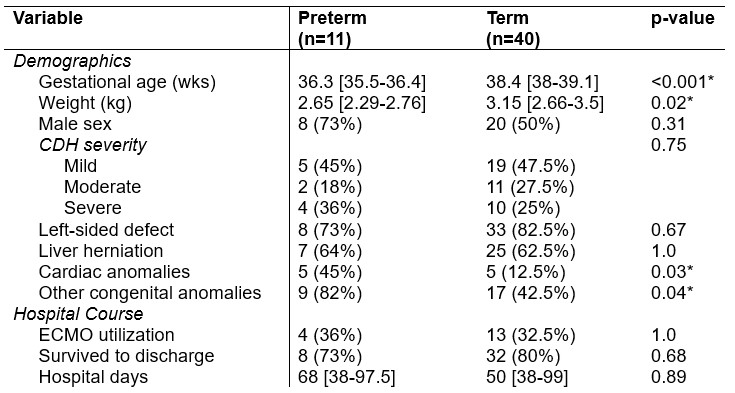 Data is represented as median [IQR] or count (%). Asterisks (*) denote results with statistical significance (p < 0.05).
Data is represented as median [IQR] or count (%). Asterisks (*) denote results with statistical significance (p < 0.05).Table 2. Transport characteristics for infants with CDH stratified by gestational age.
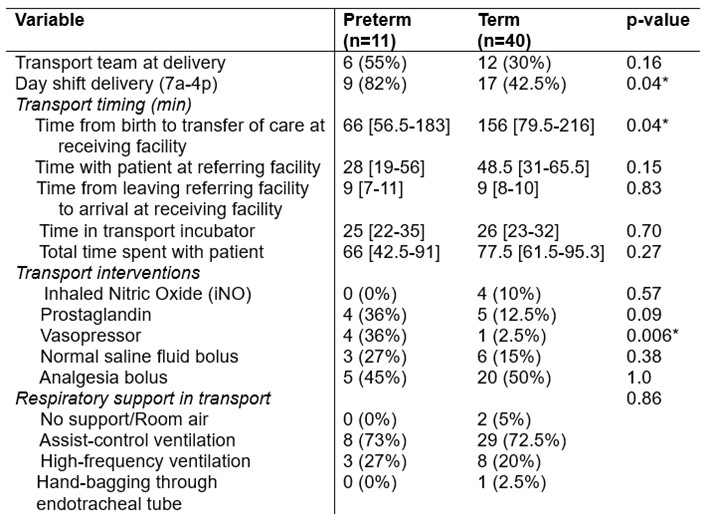 Data is represented as median [IQR] or count (%). Asterisks (*) denote results with statistical significance (p < 0.05).
Data is represented as median [IQR] or count (%). Asterisks (*) denote results with statistical significance (p < 0.05).Table 3. Number of preterm versus term infants with at least one abnormal vital sign.
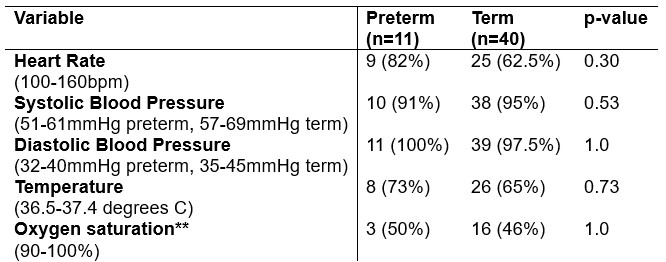 Appropriate ranges listed below each vital sign variable; any value outside of these ranges was considered abnormal. Data is represented as count (%). A single asterisk (*) denotes results with statistical significance (p < 0.05). **Oxygen saturation data removed for infants with cardiac lesions: n=5 removed preterm infants, n=5 removed term infants.
Appropriate ranges listed below each vital sign variable; any value outside of these ranges was considered abnormal. Data is represented as count (%). A single asterisk (*) denotes results with statistical significance (p < 0.05). **Oxygen saturation data removed for infants with cardiac lesions: n=5 removed preterm infants, n=5 removed term infants.Table 1. Demographics and hospital course variables for infants with CDH stratified by gestational age.
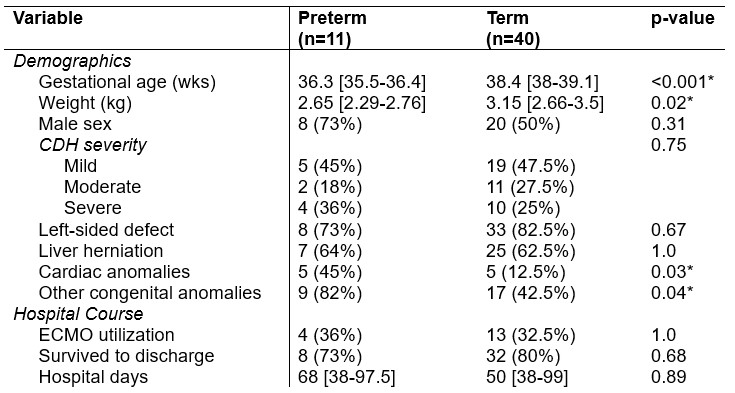 Data is represented as median [IQR] or count (%). Asterisks (*) denote results with statistical significance (p < 0.05).
Data is represented as median [IQR] or count (%). Asterisks (*) denote results with statistical significance (p < 0.05).Table 2. Transport characteristics for infants with CDH stratified by gestational age.
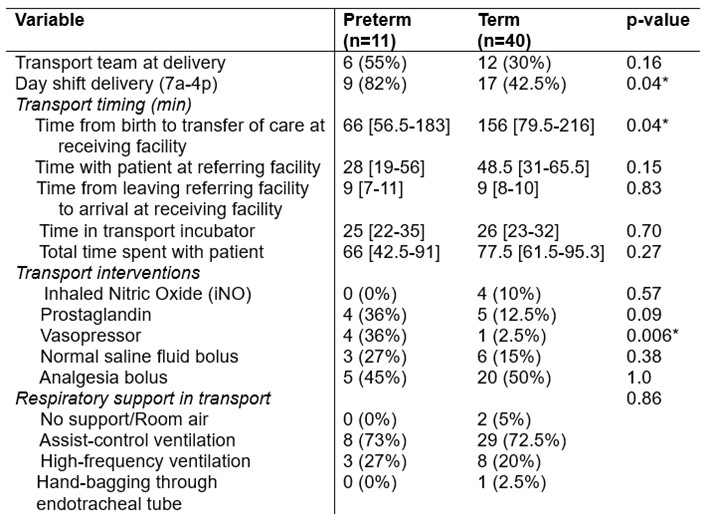 Data is represented as median [IQR] or count (%). Asterisks (*) denote results with statistical significance (p < 0.05).
Data is represented as median [IQR] or count (%). Asterisks (*) denote results with statistical significance (p < 0.05).Table 3. Number of preterm versus term infants with at least one abnormal vital sign.
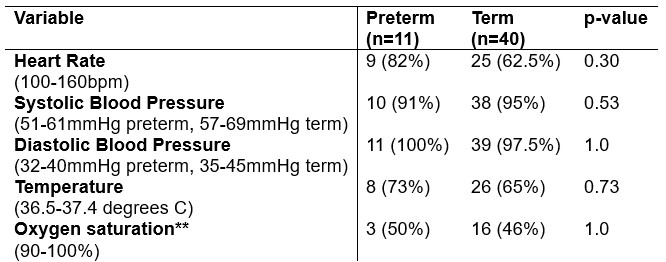 Appropriate ranges listed below each vital sign variable; any value outside of these ranges was considered abnormal. Data is represented as count (%). A single asterisk (*) denotes results with statistical significance (p < 0.05). **Oxygen saturation data removed for infants with cardiac lesions: n=5 removed preterm infants, n=5 removed term infants.
Appropriate ranges listed below each vital sign variable; any value outside of these ranges was considered abnormal. Data is represented as count (%). A single asterisk (*) denotes results with statistical significance (p < 0.05). **Oxygen saturation data removed for infants with cardiac lesions: n=5 removed preterm infants, n=5 removed term infants.
