Neonatal GI Physiology & NEC 4
Session: Neonatal GI Physiology & NEC 4
707 - Predictors of Adverse Outcomes Post-Surgical Necrotizing Enterocolitis in Preterm Neonates: A Retrospective Cohort Study
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 707.6513
Dwayne Mascarenhas, The Hospital for Sick Children, Toronto, ON, Canada; Ujjwala Mantha, The Hospital for Sick Children, Toronto, ON, Canada; Jordan Mann, The Hospital for Sick Children, Toronto, ON, Canada; Telford Yeung, University of Calgary, Calgary, AB, Canada; Mary A. Woodward, The Hospital for Sick Children, Toronto, ON, Canada; Bonny Jasani, The Hospital for Sick Children, Toronto, ON, Canada
.jpg)
Dwayne Mascarenhas, MBBS, MD (Paeds), DM (Neonatology) (he/him/his)
Clinical Fellow
The Hospital for Sick Children
Toronto, Ontario, Canada
Presenting Author(s)
Background: Surgical necrotizing enterocolitis (sNEC) is associated with devastating outcomes in preterm neonates especially mortality ranging from 40-50%. However, there is paucity of data regarding pre-operative predictors of mortality in preterm neonates with sNEC.
Objective: To identify predictors of mortality in preterm infants with sNEC.
Design/Methods: We conducted a retrospective cohort study of preterm infants ≤30 weeks with sNEC at a single quaternary neonatal intensive care unit between January 1, 2016, and June 30, 2024. Baseline characteristics, pre-operative labs, and details of sNEC management were analyzed for association with NEC-attributable mortality. Mann-Whitney U test and Fisher’s exact test were used for comparing continuous and categorical data respectively between the two groups. Multi-logistic regression analysis was conducted to evaluate the association between pre-operative (within 48 hours of surgery) variables and NEC-attributable mortality, adjusted for confounders.
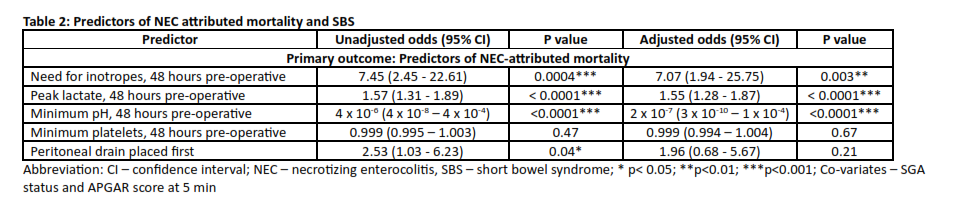
Results: Of the 139 preterm infants with sNEC, 38 (27%) neonates had NEC-attributable mortality. The baseline characteristics, details of sNEC, and pre-operative labs of preterm infants with NEC-attributable mortality versus the sNEC (n=101) who either survived (n=87) or had non NEC-related cause for mortality (n=14) are outlined in Table 1. Infants with NEC-attributable mortality had significantly lower pH, higher lactate, and need for vasopressors on univariate analysis. Post-adjusted analysis, the odds of NEC-attributable mortality were significantly higher with lower pH, higher lactate, and need for vasopressors pre-operatively (Table 2).
Conclusion(s): Our study showed that predictors of mortality secondary to sNEC in preterm neonates included pre-operative lower pH, higher lactate, and need for vasopressors.
Figure 1: Baseline and pre-operative characteristics
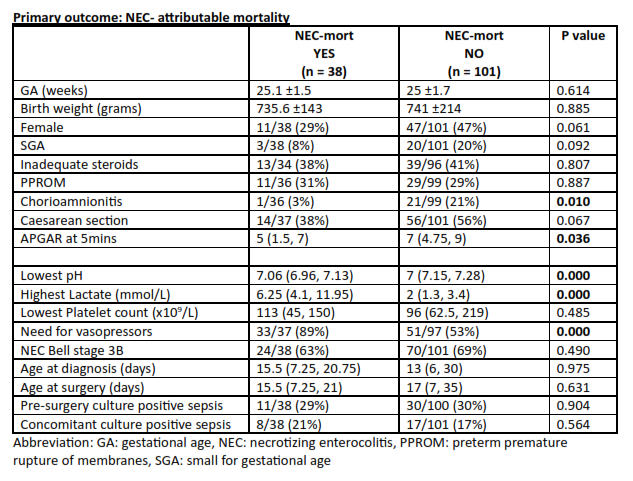
Table 2: Multivariate logistic regression: Association between pre-operative predictors and NEC-attributable mortality