Back
Background: The relationship between early life factors and childhood pulmonary function and structure in preterm infants remains unclear.
Objective: This study aims to investigate the differences in pulmonary functions between very preterm (VP) and extremely preterm (EP) infants, with and without a diagnosis of bronchopulmonary dysplasia (BPD), at school age.
Design/Methods: The LONGitudinal cohort study of the population born preterm (LONGTERM) was conducted since 2019 and has been recruiting children aged ≥5 years who were born prematurely at two tertiary center (Severance and Gangnam Severance Hospital, Seoul, Korea) for comprehensive respiratory assessment including pulmonary function testing (PFT). Participants born between 2010 and 2019 and under gestational age (GA) 32 weeks were analyzed in this study. They were divided into VP group (GA 28-31 weeks) and EP group (GA < 28 weeks). The 2019 Jensen definition was used to categorize BPD.
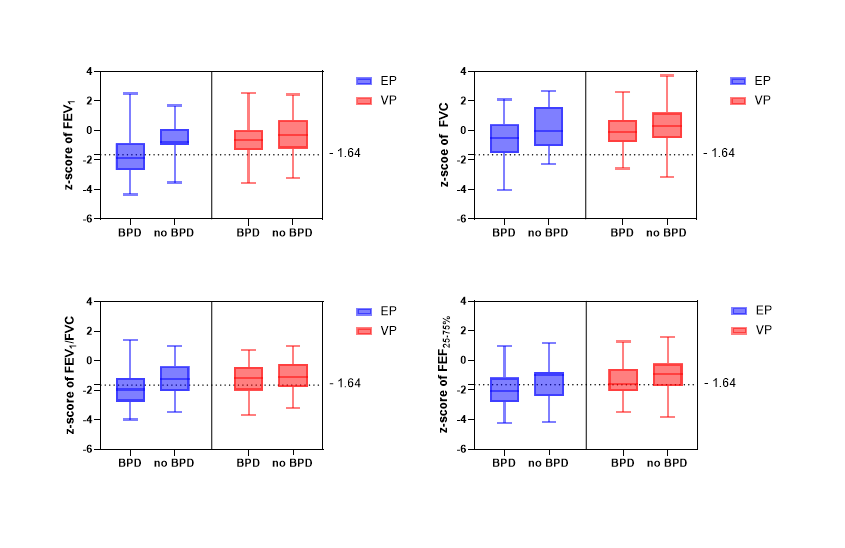
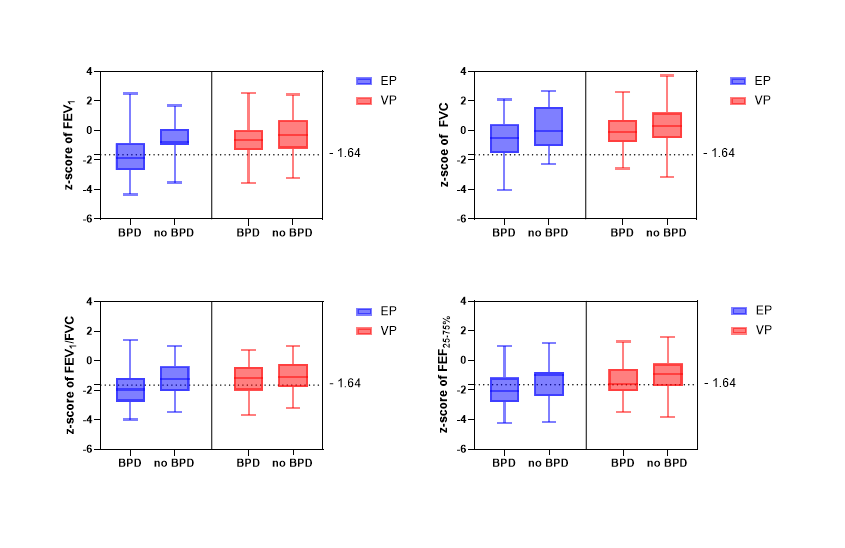
Results: Among the 206 patients (42.5% female), 78 (37.9%) were classified as EP. BPD was diagnosed in 105 patients (53.3%), with severity grades 1,2 and 3 observed in 51 (25.9%), 39 (19.8%), and 15 (7.6%) patients, respectively. PFT was performed at 7.1 ± 1.6 years. The mean z-score in FEV1, FVC, FEV1/FVC and FEF25-75% were significantly lower in the EP group comparing to the VP (-1.41 vs. -0.51, -0.50 vs. 0.30, -1.72 vs. -1.14, and -1.85 vs. -1.13, respectively, all P < 0.05). The proportion of patients with an FEV1 below the lower limit of normal (LLN) was higher in the EP group than VP group (48.7% vs 18.0%, P < 0.001), while the bronchodilator response did not differ significantly between the groups. In both the EP and VP group, patients with BPD had significantly lower mean FEV1 z-score compared to those without BPD (-1.7 vs. -0.66, P < 0.01 and -0.75 vs -0.30, P=0.049). However, the proportion of patients with FEV1 below LLN was only significantly higher in the EP group (61% vs 13%, P = 0.001). Among patients without BPD, all PFT parameters showed no significant difference between EP and VP groups.
Conclusion(s): Children born as EP showed lower PFT results and a higher prevalence of abnormal lung function compared to VP. Pulmonary function was reduced in patients with BPD compared to those without, with no significant difference between EP and VP groups in the absence of BPD. Our results indicate the importance of longitudinal monitoring and management of these vulnerable populations.
Table 1. Difference in pulmonary function test between extremely preterm infants (EP) and very preterm infants (VP)
.png)
Table 2. Difference in pulmonary function test in extremely preterm infants (EP) and very preterm infants (VP)
.png)
Figure 1. Pulmonary function test results of extremely preterm and very preterm with/without bronchopulmonary dysplasia
Neonatal Pulmonology - Clinical 6: Respiratory Concerns of the Preterm
Session: Neonatal Pulmonology - Clinical 6: Respiratory Concerns of the Preterm
377 - Differences in Pulmonary Function Among School-Aged Children Born Very Preterm and Extremely Preterm: Insights from the LONGTERM Cohort
Monday, April 28, 2025
7:00am – 9:15am HST
Joo Hi Kim, Severance Hospital, Seoul, Seoul-t'ukpyolsi, Republic of Korea; Jeong Eun Shin, Yonsei University College of Medicine, Seoul, Seoul-t'ukpyolsi, Republic of Korea; Jung Ho Han, Yonsei medical center, Seodaemoon-gu, Seoul-t'ukpyolsi, Republic of Korea; Kyung Won Kim, Yonsei University College of Medicine, Seoul, Seoul-t'ukpyolsi, Republic of Korea; Soo Yeon Kim, Yonsei University College of Medicine, Seoul, Seoul-t'ukpyolsi, Republic of Korea; Soon Min Lee, Yonsei University College of Medicine, seoul, Seoul-t'ukpyolsi, Republic of Korea; Joohee Lim, Gangnam severance hospital, Yonsei University, seoul, Seoul-t'ukpyolsi, Republic of Korea; Ho Seon Eun, Severance hospital, seoul, Seoul-t'ukpyolsi, Republic of Korea; Min Soo Park, Yonsei University College of Medicine, Seoul, Seoul-t'ukpyolsi, Republic of Korea; Ji Ye Jung, Yonsei University College of Medicine, Seoul, Seoul-t'ukpyolsi, Republic of Korea
- JK
Joo Hi Kim
Fellow
Severance Hospital
Seoul, Seoul-t'ukpyolsi, Republic of Korea
Presenting Author(s)
Background: The relationship between early life factors and childhood pulmonary function and structure in preterm infants remains unclear.
Objective: This study aims to investigate the differences in pulmonary functions between very preterm (VP) and extremely preterm (EP) infants, with and without a diagnosis of bronchopulmonary dysplasia (BPD), at school age.
Design/Methods: The LONGitudinal cohort study of the population born preterm (LONGTERM) was conducted since 2019 and has been recruiting children aged ≥5 years who were born prematurely at two tertiary center (Severance and Gangnam Severance Hospital, Seoul, Korea) for comprehensive respiratory assessment including pulmonary function testing (PFT). Participants born between 2010 and 2019 and under gestational age (GA) 32 weeks were analyzed in this study. They were divided into VP group (GA 28-31 weeks) and EP group (GA < 28 weeks). The 2019 Jensen definition was used to categorize BPD.
Results: Among the 206 patients (42.5% female), 78 (37.9%) were classified as EP. BPD was diagnosed in 105 patients (53.3%), with severity grades 1,2 and 3 observed in 51 (25.9%), 39 (19.8%), and 15 (7.6%) patients, respectively. PFT was performed at 7.1 ± 1.6 years. The mean z-score in FEV1, FVC, FEV1/FVC and FEF25-75% were significantly lower in the EP group comparing to the VP (-1.41 vs. -0.51, -0.50 vs. 0.30, -1.72 vs. -1.14, and -1.85 vs. -1.13, respectively, all P < 0.05). The proportion of patients with an FEV1 below the lower limit of normal (LLN) was higher in the EP group than VP group (48.7% vs 18.0%, P < 0.001), while the bronchodilator response did not differ significantly between the groups. In both the EP and VP group, patients with BPD had significantly lower mean FEV1 z-score compared to those without BPD (-1.7 vs. -0.66, P < 0.01 and -0.75 vs -0.30, P=0.049). However, the proportion of patients with FEV1 below LLN was only significantly higher in the EP group (61% vs 13%, P = 0.001). Among patients without BPD, all PFT parameters showed no significant difference between EP and VP groups.
Conclusion(s): Children born as EP showed lower PFT results and a higher prevalence of abnormal lung function compared to VP. Pulmonary function was reduced in patients with BPD compared to those without, with no significant difference between EP and VP groups in the absence of BPD. Our results indicate the importance of longitudinal monitoring and management of these vulnerable populations.
Table 1. Difference in pulmonary function test between extremely preterm infants (EP) and very preterm infants (VP)
.png)
Table 2. Difference in pulmonary function test in extremely preterm infants (EP) and very preterm infants (VP)
.png)
Figure 1. Pulmonary function test results of extremely preterm and very preterm with/without bronchopulmonary dysplasia