Neonatal General 11
Session: Neonatal General 11
409 - Urinary Titin as a Non-Invasive Indicator of Perinatal Distress
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 409.6830
Kazumasa Fuwa, Nihon University, Nerima-ku, Tokyo, Japan; Koh Okuda, Nihon University Itabashi Hospital, Itabashi, Tokyo, Japan; Hidetoshi Go, Nihon University School of Medicine, Itabashi, Tokyo, Japan; Midori Hijikata, Department of Pediatrics and Child Health, Nihon University School of Medicine, Itabashi-ku, Tokyo, Japan; Aya Okahashi, Nihon university school of medicine, Itabashi-ku, Tokyo, Japan; Nobuhiko Nagano, Department of Pediatrics and Child Health, Nihon University School of Medicine, Itabashi-ku, Tokyo, Japan; Ichiro Morioka, Nihon University School of Medicine, Itabashi, Tokyo, Japan
- KF
Kazumasa Fuwa, MD, PhD
Assistant professor
Nihon University
Nerima-ku, Tokyo, Japan
Presenting Author(s)
Background: Urinary titin is a protein specifically expressed in striated muscles and is a biomarker for muscle breakdown, often elevated in conditions such as Duchenne muscular dystrophy. In neonates, asphyxia is known to result in elevated muscle-derived enzymes. However, the relationship between urinary titin levels and perinatal distress remains unclear.
Objective: To examine the association between early postnatal urinary titin levels and clinical factors, including neonatal asphyxia.
Design/Methods: Neonates admitted to the NICU between 2021 and 2024 were included. Asphyxia was defined as an Apgar score below 7 at 1 min after birth. Urine samples were collected at day 0 or day 1 of life, and urinary titin levels were measured using the Titin N-Fragment Assay ELISA Kit. The relationship between the urinary titin/creatinine (Cr) ratio and clinical factors was then analyzed. Correlations between the urinary titin/Cr ratio and clinical characteristics were analyzed using 95% confidence ellipses within each group—all patients, those with asphyxia, and those without. Clinical characteristics were compared between the asphyxia and non-asphyxia groups. Finally, multiple regression analysis was used to assess the urinary titin/Cr ratio, with gestational age and CK as predictors. Statistical significance was set at p< 0.05.
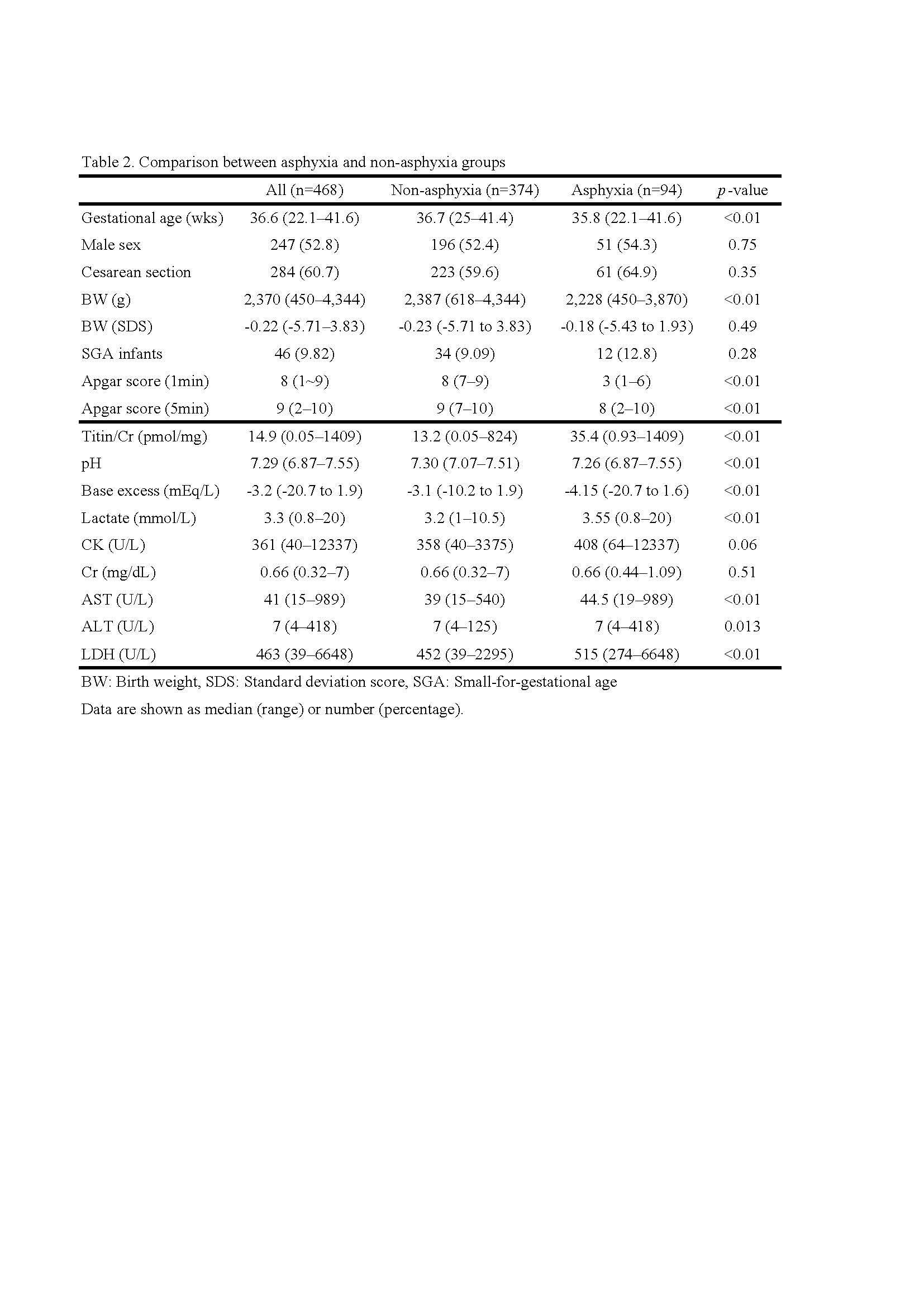
Results: Correlations between urinary titin/Cr and clinical factors are summarized in Table 1, and comparisons between infants with and without asphyxia are shown in Table 2. In all patients, urinary titin/Cr was negatively correlated with pH, base excess (BE), and gestational age and positively correlated with lactate, CK, AST, ALT, and LDH. The correlation with muscle-derived enzymes was more robust in the asphyxia group than in the overall cohort. The urinary titin/Cr ratio was significantly higher in the asphyxia group compared to the non-asphyxia group [asphyxia: 35.4 (0.93–1409) non-asphyxia: 13.2 (0.05–824), pmol/mg, p< 0.01]. Multiple regression analysis showed that CK and gestational age were independent factors associated with urinary titin/Cr (gestational age: β -0.312, SE 0.97, t -9.5, p< 0.05; CK: β 0.753, SE 0.005, t 22.92, p< 0.05), with an R² of 0.54.
Conclusion(s): Urinary titin was positively correlated with muscle-derived enzymes, showing a stronger association in cases with neonatal asphyxia, which suggests its potential as a marker of perinatal distress. Gestational age also emerged as a significant factor. Urinary titin may be a non-invasive biomarker for prenatal distress, particularly in preterm infants.
Table 1. Results of correlation analysis
.jpg)
Table 2. Comparison between asphyxia and non-asphyxia groups