Mental Health 4
Session: Mental Health 4
103 - Risk Factors for Positive Parental Postnatal Depression Screening in the NICU and at 6-9 Months
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 103.6299
Alexandra P. Russell, Creighton University School of Medicine, Omaha, NE, United States; Kerry Miller, University of Nebraska College of Medicine, Omaha, NE, United States; Cara Solness, UNMC, Omaha, NE, United States; Paige E. Hardy, Munroe-Meyer Institute, Omaha, NE, United States; Elizabeth Lyden, University of Nebraska College of Medicine, Omaha, NE, United States; Abbey Siebler, UNMC, Elkhorn, NE, United States; Brianna K.. Brei, University of Nebraska College of Medicine, Omaha, NE, United States; Eric S. Peeples, University of Nebraska Medical Center, Omaha, NE, United States

Alexandra P. Russell (she/her/hers)
Medical Student
Creighton University School of Medicine
Omaha, Nebraska, United States
Presenting Author(s)
Background: Postnatal depression affects ≥10-15% of mothers and can significantly alter maternal-infant bonding, maternal quality of life, and infant development, behavior, and overall health. Mothers and fathers of infants admitted to the newborn intensive care unit (NICU) may experience higher levels of postnatal depression and be at greater risk for these negative outcomes. However, little is known about the longitudinal post-discharge progression of postnatal depression of mothers and fathers.
Objective: To identify clinical associations with positive maternal or paternal Edinburgh Postnatal Depression Scale (EPDS) screening of NICU-hospitalized infants in-hospital, as well as risk factors for increased or stagnant maternal EPDS between NICU discharge and 6-9 months.
Design/Methods: Clinical and sociodemographic data and EPDS results were obtained from two local NICUs and a statewide high-risk infant follow-up clinic between 2014 and 2024. Infants without completed EPDS screenings at both initial hospitalization and the 6-9 month follow up visit were excluded. Demographics and early clinical outcomes were compared between parents with scores ≥10 versus < 10. Additionally, subjects were stratified by EPDS trajectory between discharge and the 6-9 month clinic visit (decreased versus unchanged/increased) and risk factors were compared between groups. A multivariable logistic regression model was generated using significant variables from univariable analysis.
Results: In this study of 258 infants, 60/258 (23%) mothers and 4/22 (18%) fathers screened positive for depression during the NICU stay. Table 1 shows demographics and neonatal outcomes stratified by positive maternal EPDS in the NICU. Non-married status, prior depression history, retinopathy of prematurity, and low gestational age were independent predictors in the regression model (Table 2). Maternal, not paternal, EPDS declined significantly from hospital to follow-up (Fig 1). EPDS scores that increased or stayed the same between hospital discharge and the 6-9 month follow up visit were associated with death of multi-birth sibling and lower 1-minute Apgar score.
Conclusion(s): Several indicators of infant health collected in the NICU were predictive of positive in-hospital EPDS screening but did not strongly predict changes in EPDS over time post-discharge, suggesting there are likely unmeasured post-discharge variables primarily driving post-discharge depression symptoms. Continued research on how postnatal depression develops over time will facilitate strategies for improved support for families and long-term outcomes.
Table 1
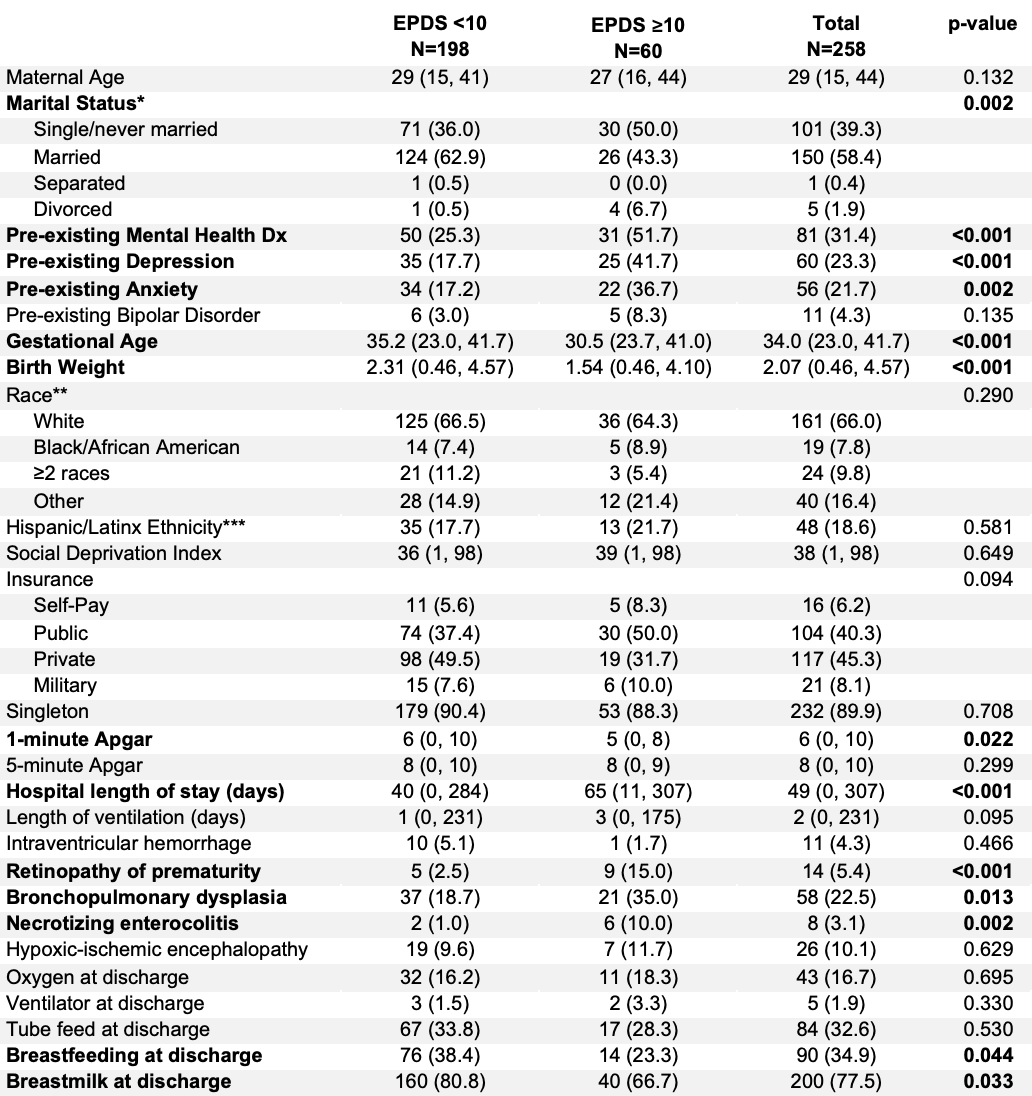 Comparison of selected maternal and infant demographics, stratified by maternal Edinburgh Postnatal Depression Scale (EPDS) score, with a score ≥10 considered to be a positive postnatal depression screening. Continuous variables are described as median (min, max); categorical as count (%). *Marital status unknown in 1 participant; **Race unknown in 14 participants; ***Ethnicity unknown in 10 participants.
Comparison of selected maternal and infant demographics, stratified by maternal Edinburgh Postnatal Depression Scale (EPDS) score, with a score ≥10 considered to be a positive postnatal depression screening. Continuous variables are described as median (min, max); categorical as count (%). *Marital status unknown in 1 participant; **Race unknown in 14 participants; ***Ethnicity unknown in 10 participants.Table 2
.png) Multivariable logistic regression predicting positive maternal Edinburgh Postnatal Depression Scale screening (≥10) during the initial neonatal intensive care unit hospitalization.
Multivariable logistic regression predicting positive maternal Edinburgh Postnatal Depression Scale screening (≥10) during the initial neonatal intensive care unit hospitalization.Figure 1
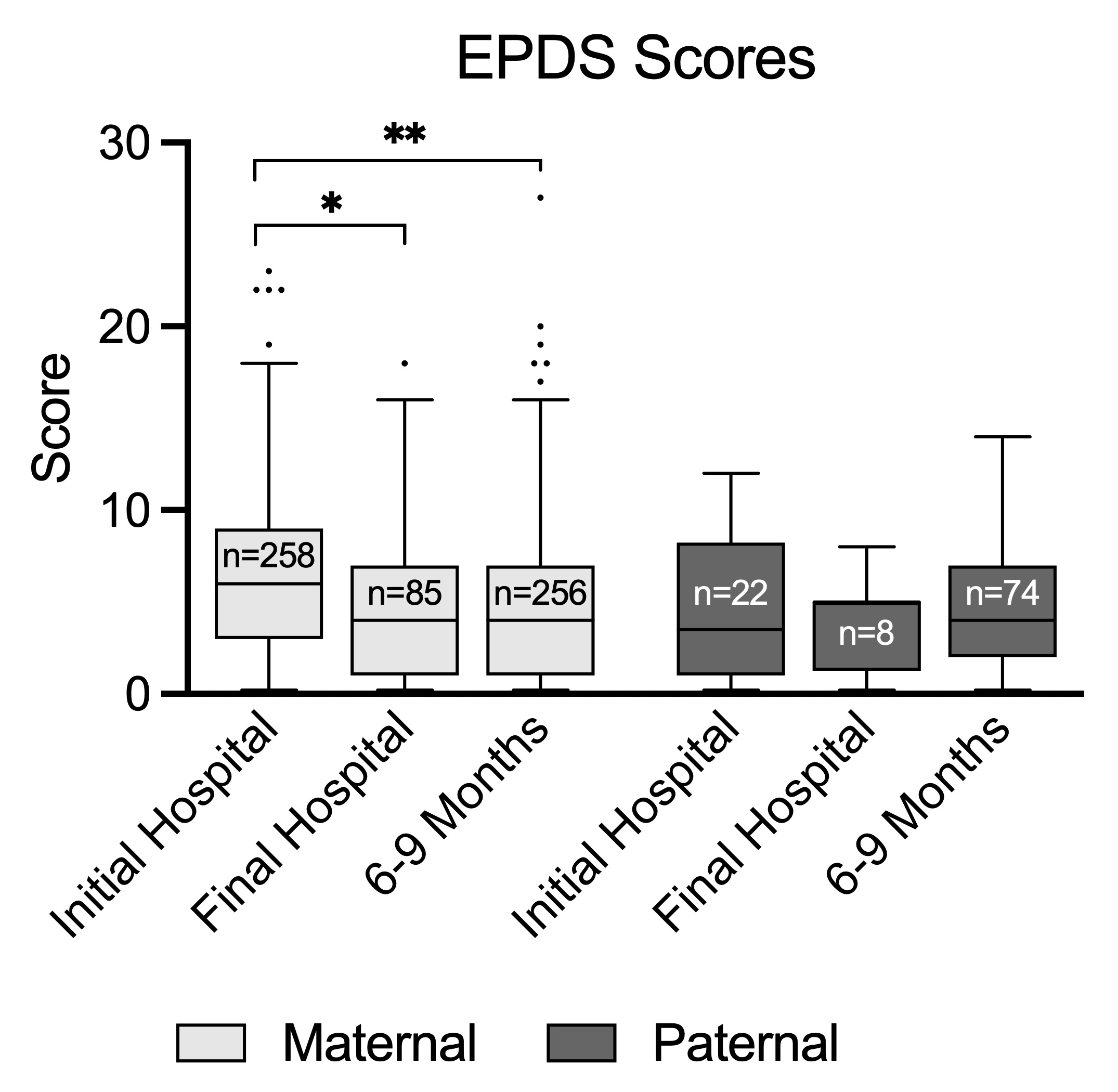 Comparison of median maternal and paternal Edinburgh Postnatal Depression Scale (EPDS) scores at time of initial in-hospital screening, final in-hospital screening (if >1 in-hospital screening performed), and 6-9 month follow up visit. Line at median and whiskers demonstrate Tukey distribution. *p < 0.05, **p < 0.0001
Comparison of median maternal and paternal Edinburgh Postnatal Depression Scale (EPDS) scores at time of initial in-hospital screening, final in-hospital screening (if >1 in-hospital screening performed), and 6-9 month follow up visit. Line at median and whiskers demonstrate Tukey distribution. *p < 0.05, **p < 0.0001
