Adolescent Medicine 5: Potpourri
Session: Adolescent Medicine 5: Potpourri
145 - Prevalence of metabolic dysfunction-associated steatotic liver disease (MASLD) and its association with arterial stiffness in adolescents: Results from the EVA4YOU study
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 145.6296
Johannes Nairz, Department of Pediatrics III, Medical University of Innsbruck, Innsbruck, Tyrol, Austria, Innsbruck, Tirol, Austria; Alex Messner, Department of Pediatrics II, Medical University of Innsbruck, Innsbruck, Austria, Innsbruck, Tirol, Austria; Sophia Kiechl, VASCage, Hochzirl Hospital, Innsbruck, Tirol, Austria; Bernhard Winder, Department of vascular surgery, Feldkirch, Vorarlberg, Austria; Ralf Geiger, Pediatric Cardiology, Medical University Innsbruck, Innsbruck, Tirol, Austria; Michael Knoflach, Medical university of innsbruck, Innsbruck, Tirol, Austria; Ursula Kiechl-Kohlendorfer, Department of Pediatrics II, Medical University of Innsbruck, Innsbruck, Tirol, Austria

Johannes Nairz, MD (he/him/his)
Trainee
Department of Pediatrics III, Medical University of Innsbruck, Innsbruck, Tyrol, Austria
Innsbruck, Tirol, Austria
Presenting Author(s)
Background: There is increasing evidence that atherosclerosis, leading to cardiovascular disease (CVD) later in life, starts early in childhood. Apart from traditional risk factors for CVD, steatotic liver disease is discussed as a further cardiovascular risk factor in adolescents, similarly as it appears to be in adults.
Objective: To determine the prevalence of metabolic dysfunction-associated steatotic liver disease (MASLD) among Middle European adolescents and its association with arterial stiffness as a marker of early vascular ageing.
Design/Methods: In the cross-sectional Early Vascular Ageing in the YOUth study, liver fat content was assessed by controlled attenuation parameter (CAP) using signals acquired by FibroScan® (Echosense, Paris, France) in 14- to 19-year-old Austrian adolescents. Arterial stiffness was determined by carotid-femoral pulse wave velocity (cfPWV) and cardiovascular risk factors by a face-to-face interview, physical examination, and fasting blood analyses. Linear regression models and one-way analysis of variance were performed to analyze the association between liver fat content, MASLD and cfPWV.
Results: A total of 1292 study participants (65.2% female) aged 17.2 ± 1.3 years were included. MASLD was detected in 62 (4.8%) adolescents. CAP value showed a significant association with cfPWV in the unadjusted model (p < 0.001) but lost its significant influence in the multivariable model after adjusting for sex, age and cardiovascular risk criteria (increased BMI or waist circumference, impaired glucose metabolism, elevated blood pressure, elevated plasma triglycerides, and decreased HDL cholesterol; Table 1; p = 0.540). In the analysis of variance, a significant increase in cfPWV was observed in adolescents with any of the five cardiovascular risk criteria for MASLD (p < 0.001), but not with the additional presence of steatotic liver disease (Figure 1; p = 0.291).
Conclusion(s): In our adolescent cohort, liver fat content and MASLD were not found to be independent predictors for early vascular ageing. Nevertheless, the determination of liver fat content can be a useful tool to identify adolescents at high risk for CVD and metabolic syndrome.
Table 1. Association between CAP value and carotid-femoral pulse wave velocity
.png) Linear regression models. Model 1 is unadjusted. Model 2 with adjustment for sex and age. Model 3 with adjustment for sex, age, and the cardiometabolic risk criteria for MASLD (BMI ≥ 85th percentile or waist circumference > 95th percentile; Fasting serum glucose ≥ 5.6 mmol/L or serum glucose ≥ 11.1 mmol/L or 2-hour post-load glucose levels ≥ 7.8 mmol or glycated hemoglobin (HbA1c) ≥ 5.7% or already diagnosed/treated type 2 diabetes; Blood pressure ≥ 130/85 mmHg or specific antihypertensive drug treatment; Plasma triglycerides ≥ 1.70 mmol/L or lipid lowering treatment; Plasma high-density lipoprotein cholesterol ≤ 1.0 mmol/L or lipid lowering treatment).
Linear regression models. Model 1 is unadjusted. Model 2 with adjustment for sex and age. Model 3 with adjustment for sex, age, and the cardiometabolic risk criteria for MASLD (BMI ≥ 85th percentile or waist circumference > 95th percentile; Fasting serum glucose ≥ 5.6 mmol/L or serum glucose ≥ 11.1 mmol/L or 2-hour post-load glucose levels ≥ 7.8 mmol or glycated hemoglobin (HbA1c) ≥ 5.7% or already diagnosed/treated type 2 diabetes; Blood pressure ≥ 130/85 mmHg or specific antihypertensive drug treatment; Plasma triglycerides ≥ 1.70 mmol/L or lipid lowering treatment; Plasma high-density lipoprotein cholesterol ≤ 1.0 mmol/L or lipid lowering treatment).CAP, controlled attenuation parameter; and MASLD, metabolic dysfunction-associated steatotic liver disease.
Figure 1. Boxplot mean cfPWV comparisons.
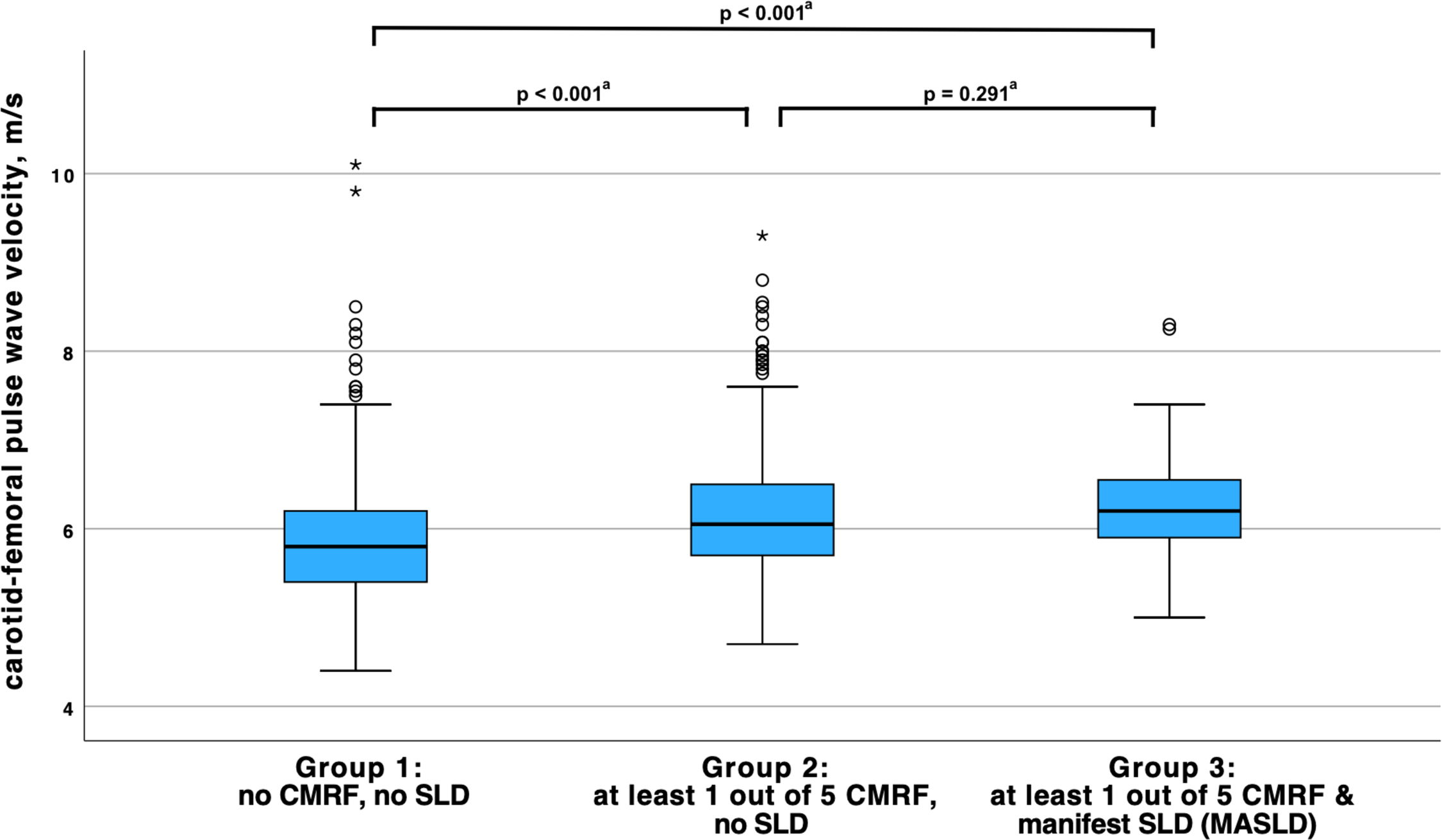 Subjects with an underlying causal liver pathology for SLD (including excessive alcohol consumption) were excluded from this analysis (N = 51), thus participants from group 3 met all definition criteria for MASLD. Moderate outliers are marked with circles (o) and extreme outliers are marked with asterisks (*). CMRF, cardiometabolic risk factor; SLD, steatotic liver disease; and MASLD, metabolic dysfunction-associated steatotic liver disease.
Subjects with an underlying causal liver pathology for SLD (including excessive alcohol consumption) were excluded from this analysis (N = 51), thus participants from group 3 met all definition criteria for MASLD. Moderate outliers are marked with circles (o) and extreme outliers are marked with asterisks (*). CMRF, cardiometabolic risk factor; SLD, steatotic liver disease; and MASLD, metabolic dysfunction-associated steatotic liver disease.a Pairwise comparison of the means using post-hoc Bonferroni statistical tests (one-way ANOVA).

