Critical Care 3
Session: Critical Care 3
493 - Routine Chest X-rays in Critical Bronchiolitis Do Not Improve Outcomes
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 493.6344
Da-Eun Choi, Loma Linda University Children's Hospital, Riverside, CA, United States; Caroline LaFerla, Loma Linda University Children's Hospital, Redlands, CA, United States; Trisha Sunderajan, Loma Linda University Children’s Hospital, Loma Linda, CA, United States; Michael Mount, UH Rainbow Babies & Children's Hospital, Cleveland, OH, United States; Harsha Chandnani, Loma Linda University Children's Hospital, Loma Linda, CA, United States; Robert D. Guglielmo, Loma Linda University Children's Hospital, Loma Linda, CA, United States; Harmanpreet S. Chawla, Loma Linda University Children's Hospital, LOMA LINDA, CA, United States; Michael Giang, Loma Linda University Children's Hospital, Loma Linda, CA, United States

Da-Eun Choi, D.O.
Chief Resident
Loma Linda University Children's Hospital
Riverside, California, United States
Presenting Author(s)
Background: Although routine chest X-rays (CXR) are not recommended by the American Academy of Pediatrics in bronchiolitis, they continue to be a mainstay in diagnostics.
Objective: We aimed to understand the impact of obtaining CXRs on clinical management in critical bronchiolitis, specifically assessing intensive care unit length of stay (ICU-LOS) and intensive care unit level of respiratory support (ICU-LRS) in patients admitted to the Pediatric intensive care unit (PICU).
Design/Methods: This single-center retrospective cohort study assessed children less than three years of age admitted to the PICU, pediatric step-down ICU and/or pediatric cardiac ICU with ICU-LRS. ICU-LRS was defined as requiring high-flow nasal cannula therapy, non-invasive mechanical ventilation, or invasive mechanical ventilation. The groups were divided into those who received or did not receive a CXR for primary analysis. The critical bronchiolitis score (CBS), a validated metric for illness severity, was used to calculate a predicted ICU-LOS and ICU-LRS. The primary outcome was the difference between actual and predicted ICU-LOS and ICU-LRS compared between the two groups.
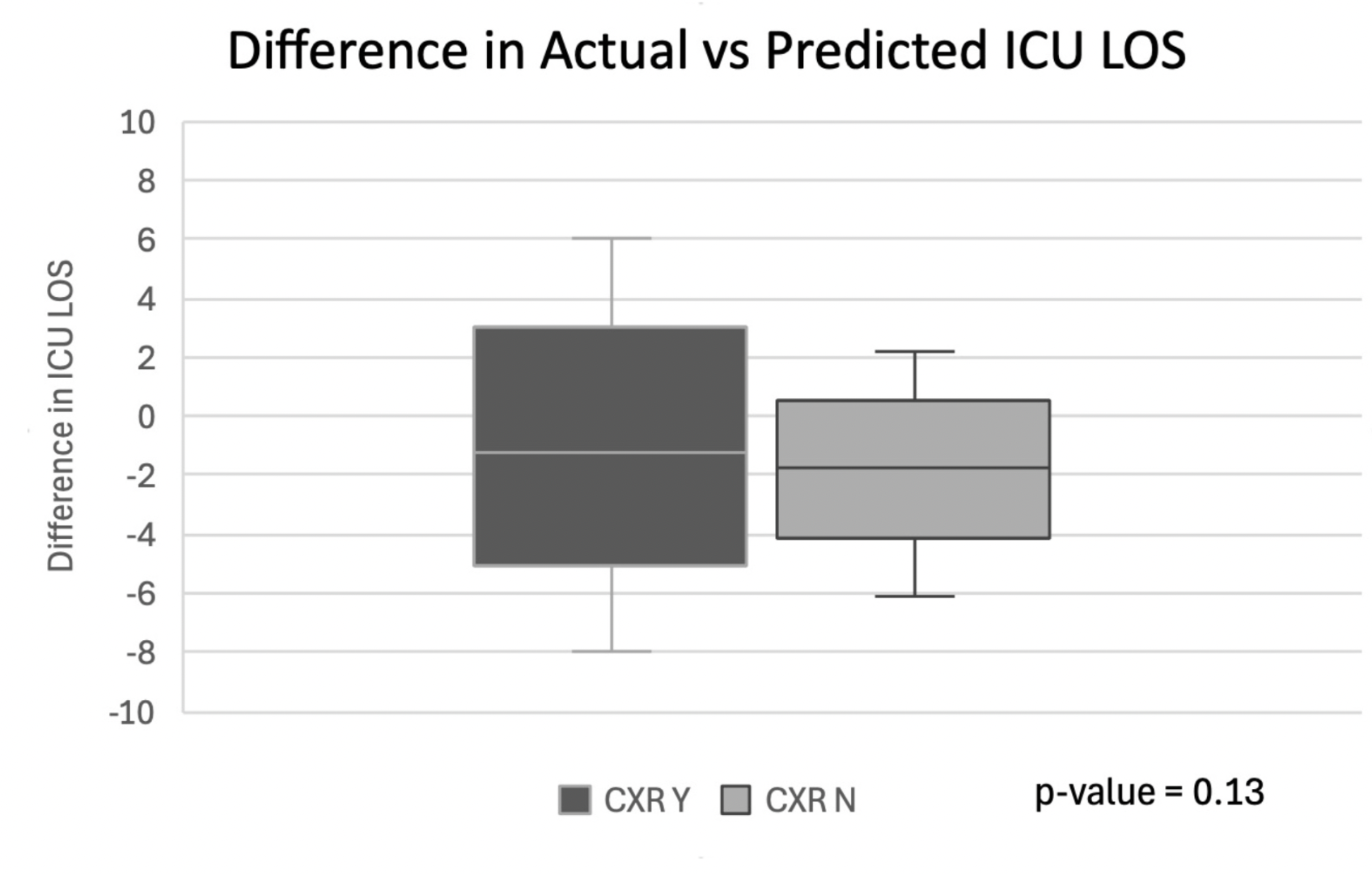
Results: 448 patients were screened from 2021-2022, with 107 meeting the inclusion criteria (demographics in figure 1). 65 of the 107 patients (60%) received a CXR with 8 (12%) having actionable CXR findings (75% obvious consolidation, 25% effusion). There was no significant difference in illness severity, with predicted median ICU-LOS and ICU-LRS of 3.5 days and 2.7 days, respectively, in the CXR group versus 3.3 days and 2.6 days in the no-CXR group (p = 0.43 and p=0.31). Actual length of stay and respiratory support were significantly shorter than predicted in all groups (Figure 2). Patients in the no-CXR group had significantly shorter actual ICU-LOS (p = 0.025) and ICU-LRS (p = 0.018) than the CXR group. The difference in median ICU-LRS and median ICU-LOS (actual minus predicted) in the CXR group of -0.6 days and -1.2 days, respectively, versus -1.0 days and -1.7 days in the no-CXR group was marginal (p=0.129 and p=0.126) (Figure 3).
Conclusion(s): Obtaining a CXR in critically ill patients with bronchiolitis did not significantly impact ICU-LOS or ICU-LRS, even when controlling for severity of illness.
Figure 1
PNG image.jpeg
Figure 2
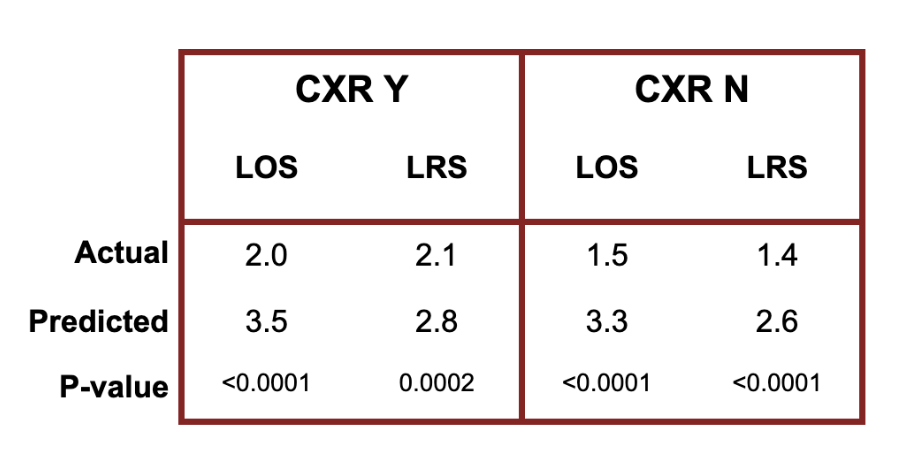
Figure 3