Emergency Medicine 14
Session: Emergency Medicine 14
573 - Project ADIOS: A Discharge Initiative of Spanish-speakers
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 573.6254
Claudia M. Fontes, Cohen Children's Medical Center, Astoria, NY, United States; Kimberly A. Giusto, Northwell Health, Rockville Centre, NY, United States; Anita Pillai, Cohen Children's Medical Center, New Hyde Park, NY, United States; Ronak Patel, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Queens, NY, United States

Claudia M. Fontes, MD (she/her/hers)
Pediatric Emergency Medicine Fellow
Cohen Children's Medical Center
Astoria, New York, United States
Presenting Author(s)
Background: Effectively communicating healthcare information to patients with limited English proficiency, especially Spanish-speaking families, is crucial in ensuring high-quality care and improving health outcomes. Language barriers can lead to misunderstandings of medical instructions, decreased adherence to treatment plans, and increased risk of adverse events.
Objective: Our aim was to improve the percentage of Spanish speaking families receiving written discharge instructions in Spanish by 50% over a five-month period in our pediatric emergency department (PED).
Design/Methods: Using a quality improvement model, an interdisciplinary team was formed to implement targeted interventions using Plan-Do-Study-Act (PDSA) cycles. A cohort of Spanish speaking patients discharged from our PED were surveyed to identify areas for improvement, such as updating discharge instructions and increasing interpreter use at discharge(pre-data). In PDSA 1, we translated discharge instructions for common diagnoses into Spanish and integrated them into the electronic medical record using acronym expanders. PDSA 2 focused on educating staff through meetings and emails. In PDSA 3, we oriented new rotating residents in the PED about the initiative, encouraging the use of acronym expanders. PDSA 4 involved the distribution of an infographic flier detailing access to acronym expanders and instructions for creating personalized Spanish discharge instructions using an institutional AI program. Post-discharge surveys were conducted to assess the new discharge experience.
Results: In our pre-data period we surveyed 44 patients. From May 2024 through September 2024 (study period), 265 discharged Spanish-speaking patient families were surveyed. We saw a significant improvement in the percentage of Spanish-speaking patients who received translated discharge instructions increasing from 43% to 82% (p = < 0.001) and use of an interpreter during the discharge process from 72% to 94% (p = 0.001) in the 5-month period. However, this did not lead to a significant increase in the percentage of patients understanding their discharge instructions.
Conclusion(s): Interventions targeting improvement in Spanish written instructions demonstrated an increased percentage of families receiving language appropriate instructions. Although not the main objective of the study, interpreter use at discharge also improved. However, further research is needed to identify potential challenges in understanding discharge instructions both during and after the discharge process.
Table 1
.png) Discharge Instructions in Spanish
Discharge Instructions in SpanishTable 2
.png) Interpreter Use at Discharge
Interpreter Use at DischargeTable 3
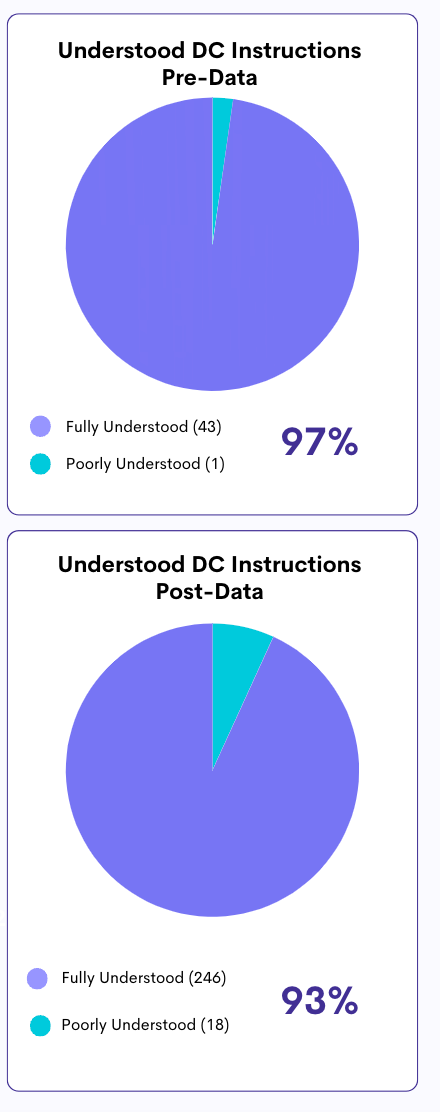 Understanding of Discharge Instructions
Understanding of Discharge Instructions
