Health Equity/Social Determinants of Health 11
Session: Health Equity/Social Determinants of Health 11
220 - The Association Between Social Distancing and Neonatal & Infant Mortality During the COVID-19 Pandemic in the United States by Social Risk Factors
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 220.6626
Denita Lindsey, University of Alabama School of Medicine, Trussville, AL, United States; Avinash Singh, Children's of Alabama, Birmingham, AL, United States; Lucinda J. Weaver, Monument Health, Rapid City, SD, United States; Arie Nakhmani, University of Alabama at Birmingham, Birmingham, AL, United States; Colm P. Travers, UAB, Birmingham, AL, United States; Rachel Sinkey, University of Alabama at Birmingham, Birmingham, AL, United States; Namasivayam Ambalavanan, University of Alabama School of Medicine, Birmingham, AL, United States; Waldemar Carlo, UAB School of Medicine, Birmingham, AL, United States; Vivek Shukla, University of Alabama at Birmingham, Birmingham, AL, United States

Denita Lindsey, MD (she/her/hers)
Fellow
University of Alabama School of Medicine
Trussville, Alabama, United States
Presenting Author(s)
Background: Neonatal mortality is an important public health challenge that disproportionately affects individuals with social risk factors associated with race, level of education, and type of insurance. Additionally, the COVID-19 pandemic exacerbated existing disparities. Social distancing measures may have led to decreased access to or utilization of health care resources, particularly among high risk groups. To better prepare for future crises, it is essential to study the association between pandemic public health interventions and mortality rates in these vulnerable groups.
Objective: To test the hypothesis that increased social distancing during the COVID-19 pandemic was associated with disproportionately higher neonatal mortality rates for individuals with social risk factors.
Design/Methods: This US population-level cohort study utilizes data from the National Center for Health Statistics (NCHS) maternal linked-birth and infant death records from 2016 through 2020. The mortality rates were correlated with the social distancing index (SDI) using machine learning based ARIMA models and lag analyses by maternal race, maternal education, and payment source subgroups. The reference period was January 2016 through February 2020; the pandemic period was defined as March through December 2020. The primary outcome was neonatal mortality rate. The secondary outcomes were early neonatal mortality and infant mortality rates.
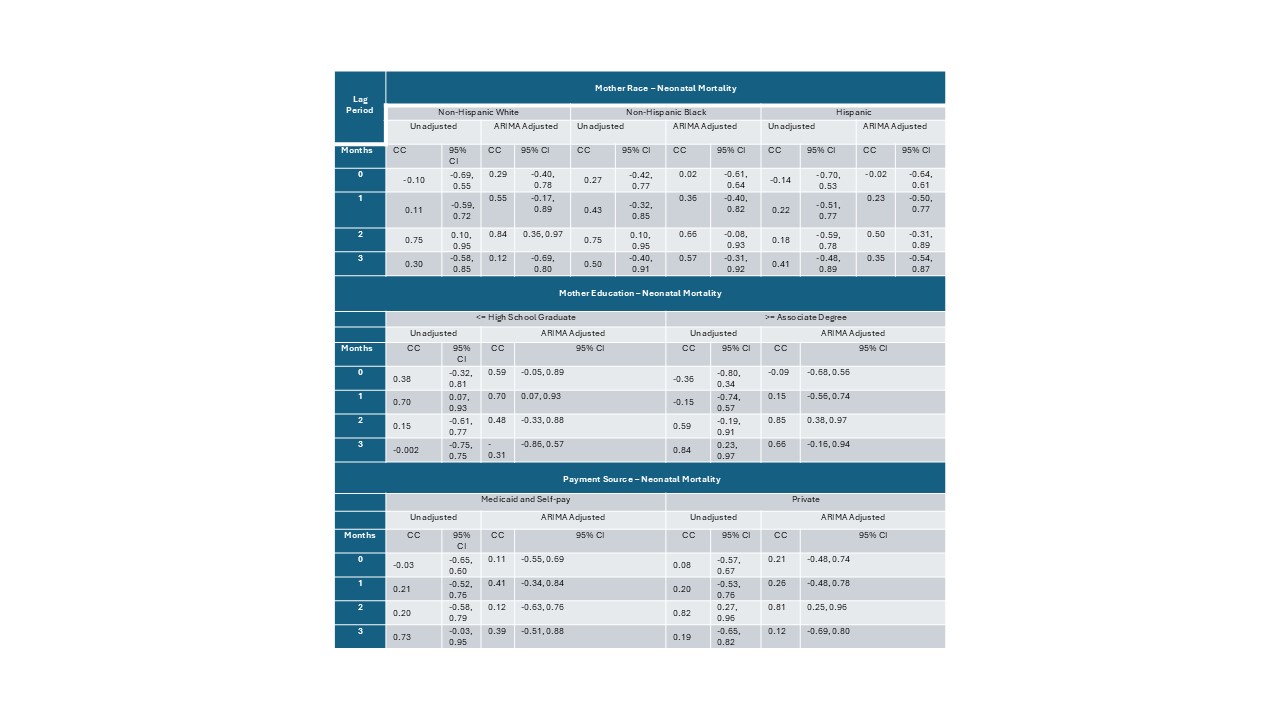
Results: A total of 18,011,173 births were analyzed, with 15,136,596 from the reference period and 2,874,577 from the pandemic period. Demographic differences were observed between the groups, as expected for a population based study with a large sample size (Table 1). Early neonatal, neonatal, and infant mortality rates were lower during the pandemic, consistent with the trend of declining mortality (Table 1). ARIMA-adjusted analysis showed no significant correlation with SDI (Figure). Lag analysis indicated SDI was linked to higher neonatal mortality, with a 1-month lag for the lower education subgroup and a 2-month lag for non-Hispanic White, higher education, and private insurance subgroups (Table 2).
Conclusion(s): The study highlights the potential associations of social distancing measures with infant health by social risk factors. The results showed there was no increase in neonatal mortality in subgroups with social risk factors.
Table 1: Baseline Characteristics and Outcomes
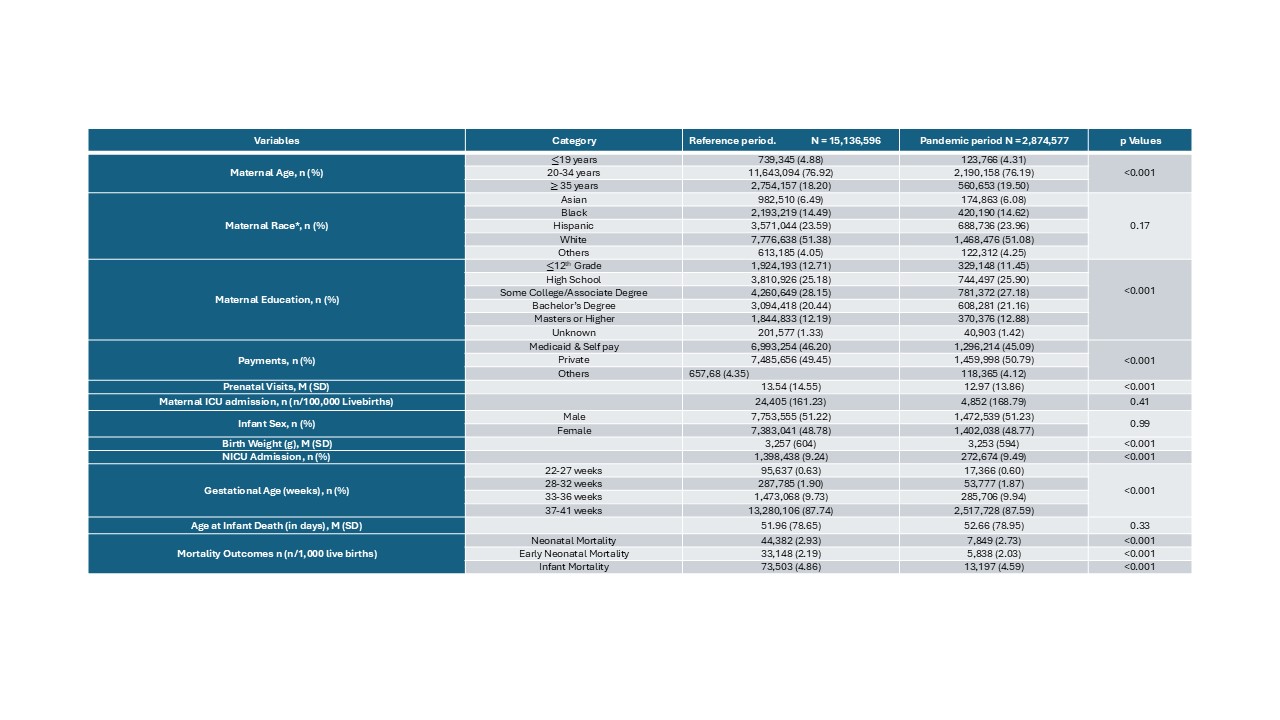 *Maternal race categories were based on self-reported race. Non-Hispanic AIAN, Non-Hispanic NHOPI, Non-Hispanic more than one race and Origin unknown or not stated in the “Others” subcategory.
*Maternal race categories were based on self-reported race. Non-Hispanic AIAN, Non-Hispanic NHOPI, Non-Hispanic more than one race and Origin unknown or not stated in the “Others” subcategory.Figure: Social Distancing Index and Percentage Change in Neonatal Mortality by Maternal Race, Maternal Education, and Payment Source
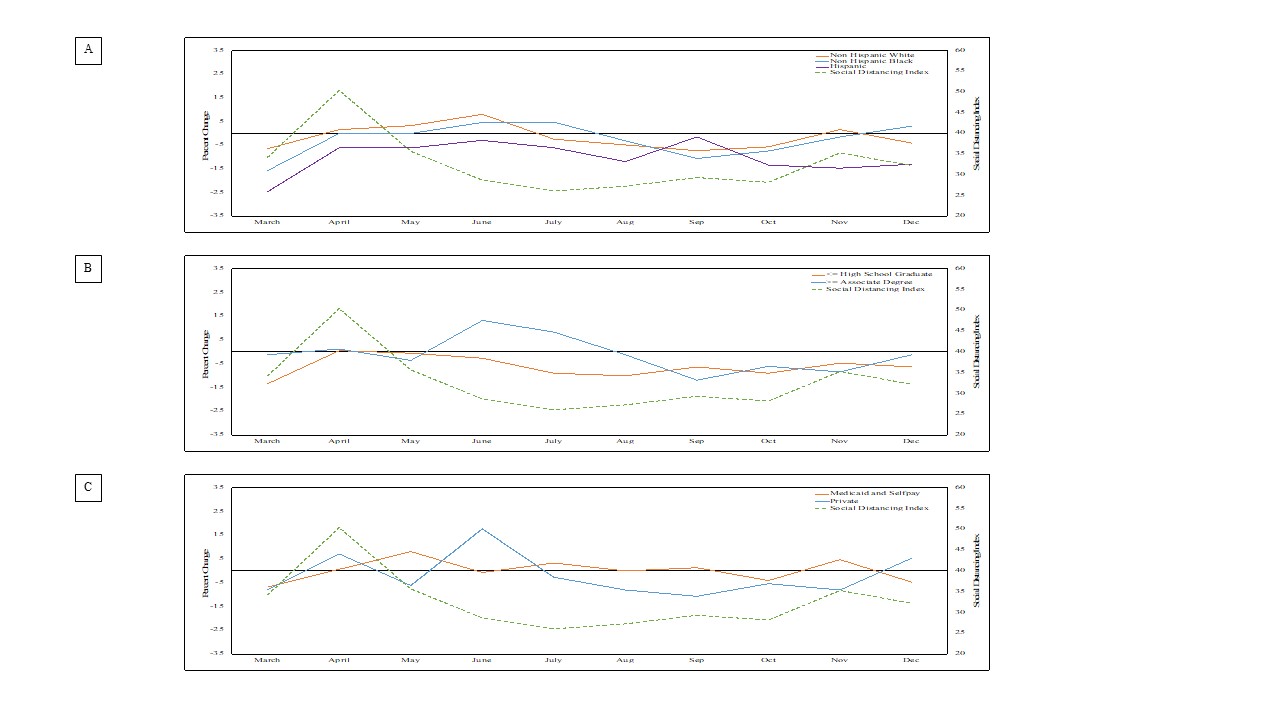 The figure shows the correlation of the social distancing index with the percent change in the autoregressive integrated moving average (ARIMA) adjusted expected neonatal mortality rates during the pandemic and reference period by subgroups: maternal race, maternal education, and payment source (panels A, B, and C respectively).
The figure shows the correlation of the social distancing index with the percent change in the autoregressive integrated moving average (ARIMA) adjusted expected neonatal mortality rates during the pandemic and reference period by subgroups: maternal race, maternal education, and payment source (panels A, B, and C respectively).Table 2: Lag Period Unadjusted Analysis of Correlation of Social Distancing Index with Neonatal Mortality