Health Equity/Social Determinants of Health 8
Session: Health Equity/Social Determinants of Health 8
177 - The impact of neighborhood-level social determinants of health on pediatric appendicitis outcomes within an integrated healthcare system
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 177.6648
Emily Kragel, Kaiser Permanente - Oakland Medical Center, Oakland, CA, United States; Priya Bhattacharjee, Kaiser Permanente - Oakland Medical Center, Oakland, CA, United States; Morah Brown, Kaiser Permanente Division of Research, Pleasanton, CA, United States; Julia Wei, Kaiser Permanente Division of Research, Pleasanton, CA, United States; Miranda Weintraub, Kaiser Permanente Oakland Medical Hospital, Oakland, CA, United States; Sani Z. Yamout, The permanente medical group, Oakland, CA, United States

Emily Kragel, MD (she/her/hers)
Chief Resident
Kaiser Permanente - Oakland Medical Center
Oakland, California, United States
Presenting Author(s)
Background: Social determinants of health (SDOH) significantly influence health outcomes. Appendicitis is the most common pediatric surgical emergency and provides a valuable model for evaluating the impact of SDOH on outcomes. Delays in medical intervention for pediatric appendicitis are strongly linked to perforation rates and related adverse outcomes. Research suggests that SDOH not only delay care-seeking but also affect in-hospital treatment and readmission risks.
Objective: To assess whether an integrated healthcare model mitigates the impact of SDOH burden—measured by neighborhood deprivation index (NDI)—on pediatric appendicitis outcomes, specifically presentation with complicated appendicitis, hospitalization duration, and readmission risk.
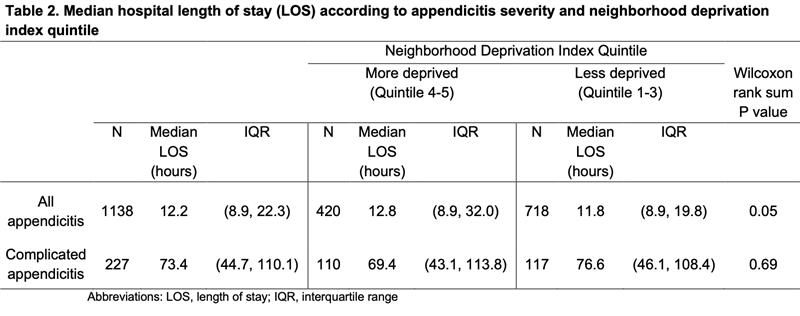
Design/Methods: This multicenter, retrospective cohort study included pediatric members of Kaiser Permanente Northern California who underwent appendectomy for acute appendicitis between January 1, 2022, and June 30, 2023. Patients were categorized by NDI into more deprived and less deprived SDOH groups. Demographic and clinical data were analyzed. Logistic regression models adjusted for relevant covariates assessed the association between NDI and complicated appendicitis, as well as readmission risk. Hospital length of stay comparisons for those with complicated appendicitis were conducted using the Wilcoxon rank-sum test.
Results: The study included 1138 pediatric patients aged 2-18 years who underwent appendectomy for acute appendicitis. Complicated appendicitis occurred in 20.0% of cases. Patients in the more deprived group (36.9%) exhibited a higher risk of complicated appendicitis, with an adjusted odds ratio (OR) of 1.6 (95% confidence interval [CI] 1.2-2.2). Complicated appendicitis occurred in 26.2% of the more deprived group compared to 16.3% in the less deprived group (p < 0.01). Among patients with complicated appendicitis, no statistically significant differences were observed in hospital length of stay or in 30-day emergency department and hospital readmission rates. Additionally, readmission odds for the more deprived group were not significantly higher (adjusted OR 1.1, 95% CI 0.5-2.3).
Conclusion(s): In this integrated healthcare system, an elevated risk of complicated appendicitis was associated with SDOH burden. However, outcomes related to length of stay and readmission risk were comparable across SDOH groups. Further research is warranted to investigate potential disparities in pre-hospitalization care for pediatric appendicitis.
Patient demographic and clinical characteristics
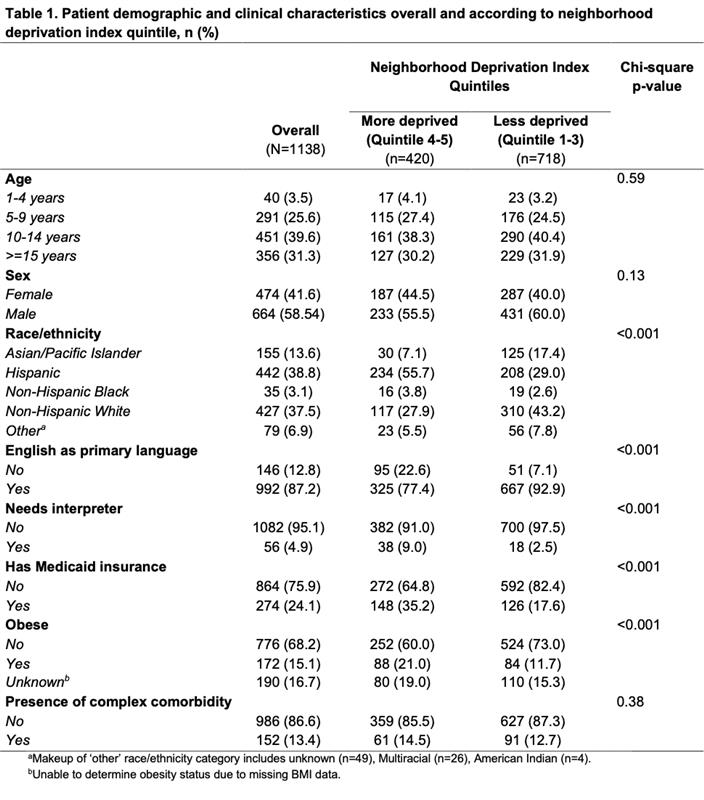
Hospital length of stay according to appendicitis severity and neighborhood deprivation index group