Mental Health 4
Session: Mental Health 4
095 - Characteristics of Pediatric Mental Health Emergency Department Visits, Transfers, and Admissions in California Prior to, During, and After the COVID-19 Pandemic
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 95.4334
Victoria T. Chi, Lucile Packard Children's Hospital Stanford, Mountain View, CA, United States; Hurnan Vongsachang, University of California, Los Angeles David Geffen School of Medicine, Los Angeles, CA, United States; Nancy Ewen Wang, Stanford University School of Medicine, Palo Alto, CA, United States
.jpg)
Victoria T. Chi, MD (she/her/hers)
Resident
Lucile Packard Children's Hospital Stanford
Mountain View, California, United States
Presenting Author(s)
Background: The COVID-19 pandemic exacerbated the pediatric mental health (MH) crisis. Less is known on whether these effects have persisted after the pandemic. Emergency department (ED) visits can be used to assess MH burden and access to MH care.
Objective: To assess rates and characteristics of pediatric MH ED visits and admissions/transfers in the pre-pandemic, pandemic, and post-pandemic periods.
Design/Methods: We performed a retrospective secondary data analysis of the California Department of Health Care Access and Information Emergency Discharge database. We examined ED visits with a primary MH diagnosis. MH visits were categorized by ICD-10 codes, and demographic data were extracted from the database. Disposition was categorized as discharge vs hospital admission or transfer to a psychiatric facility, as a proxy for severity. We examined pre-pandemic (3/1/2017-3/16/2020), pandemic (3/17/2020-8/31/2021), and post-pandemic (9/1/2021-12/21/2022) periods. Our regression models examined odds of MH ED visits, adjusting for demographic variables.
Results: The pandemic was associated with an increase in MH ED visits (OR 1.45, 95% CI 1.44-1.47), compared to pre-pandemic. The post-pandemic period saw a decrease compared to pandemic rates, but was associated with a greater odds of MH visits compared to the pre-pandemic period (OR 1.06, 95% CI 1.05-1.07). For all time periods, the most common MH visit diagnosis was suicide attempt or ideation, followed by mood disorder, anxiety, and substance use. Demographic trends were similar across all time periods, with lower odds of MH visits for male, Black, Asian, Spanish-speaking, and publicly insured patients. Odds of MH visits were higher for patients with higher socioeconomic status or living in rural areas. Rates of admissions/transfers increased during the pandemic (OR 1.17, 95% CI 1.14-1.19), compared to pre-pandemic. Odds of admissions/transfers during the post-pandemic period (OR 0.99, 95% CI 0.96-1.01) were comparable to the pre-pandemic period.
Conclusion(s): We found an increased likelihood of MH ED visits and admissions/transfers during the pandemic, compared to pre-pandemic. These findings may be explained by increased prevalence and severity of MH conditions, or decreased access to outpatient MH care. Post-pandemic, rates of MH ED visits were not as high as during the pandemic, but there was a persistent increase compared to pre-pandemic. Demographic trends remained similar across all time periods. Overall, there appears to be an ongoing mental health crisis, and further research and work must be done to ensure improved and equitable access to mental health care.
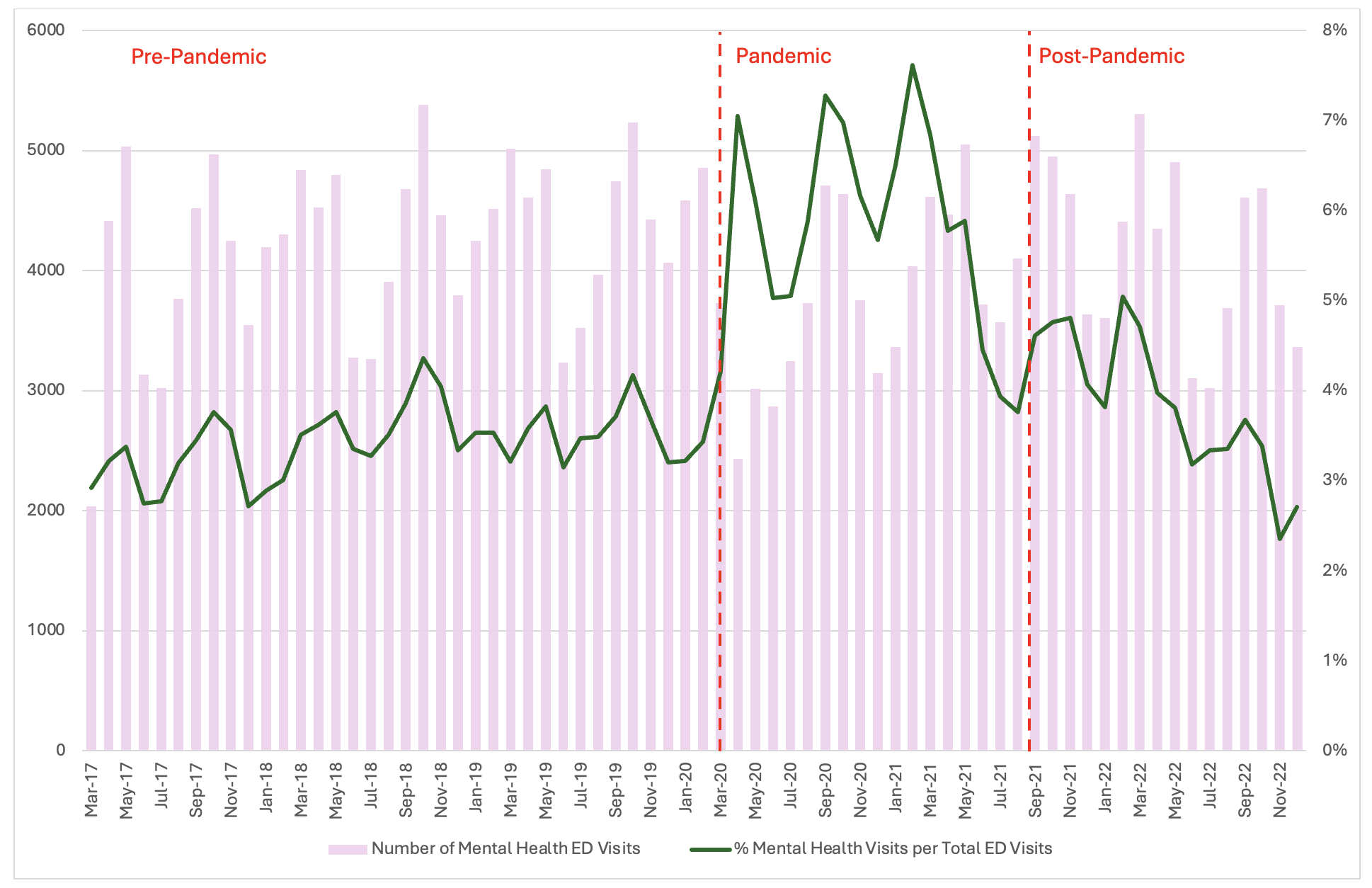
Number and percentage of ED visits with a primary mental health diagnosis per month
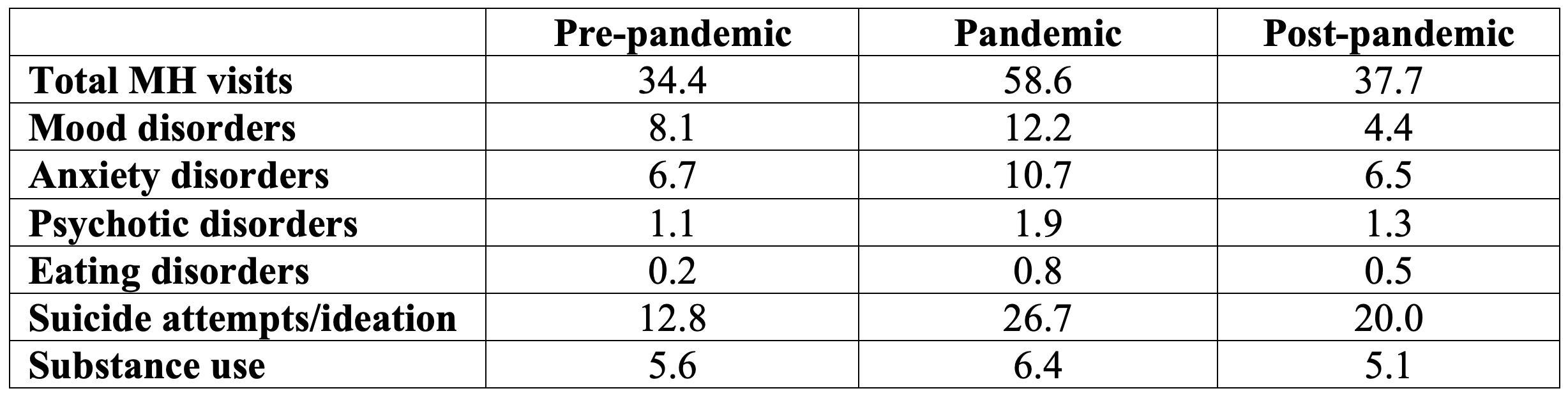
Mental health visits among children aged 6-17 per thousand ED visits, by mental health diagnosis
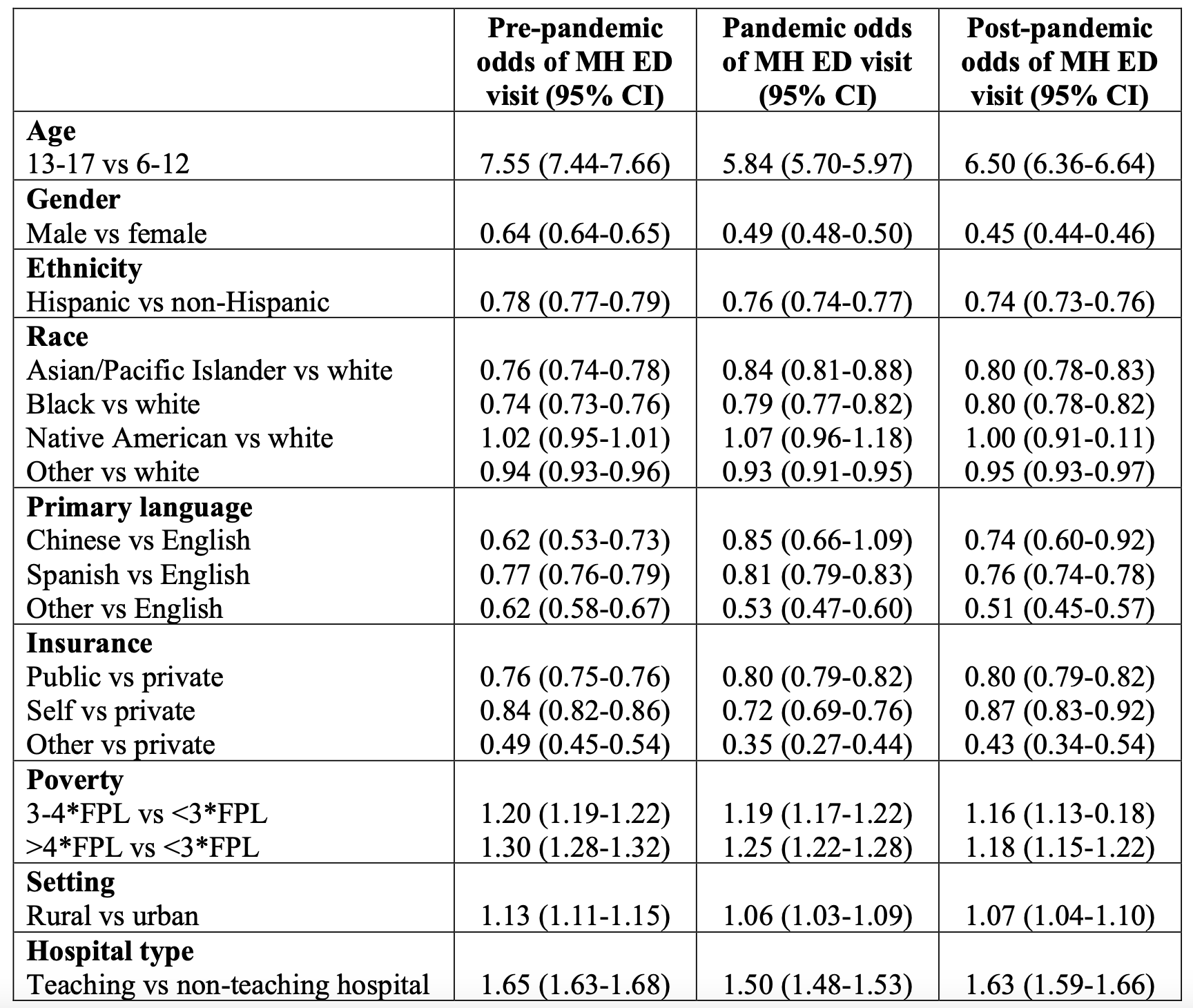
Regression analysis of demographic factors associated with pediatric mental health ED visits