Critical Care 3
Session: Critical Care 3
489 - Diabetic Ketoacidosis and Hospital-Acquired Venous Thromboembolism in Children and Young Adults
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 489.4238
Kristin M. DeMayo, USF Health Morsani College of Medicine, st. petersburg, FL, United States; Elizabeth Havlicek, University of Utah, Primary Children's Hospital, Salt Lake City, UT, United States; Jamie C. Palumbo, VPS, LLC, Pasadena, CA, United States; Gerardo Soto-Campos, VPS, LLC, Los Angeles, CA, United States; Marisol Betensky, Johns Hopkins All Children’s Hospital, St Petersburg, FL, United States; Neil Goldenberg, Johns Hopkins University School of Medicine, St. Petersburg, FL, United States; Anthony A. Sochet, Johns Hopkins All Children's Hospital, St. Petersburg, FL, United States

Kristin M. DeMayo, DO (she/her/hers)
Resident Physician
USF Health Morsani College of Medicine
st. petersburg, Florida, United States
Presenting Author(s)
Background: Those hospitalized for diabetic ketoacidosis (DKA) are thought to be at increased risk of venous thromboembolism (VTE) as a result of hyperosmolarity and acidosis. The frequency of VTE and associated risk factors are not reported in pediatrics.
Objective: To estimate the occurrence rate of hospital-acquire (HA)-VTE in critically ill children and young adults using a multicenter, North American database and evaluate putative DKA-related prothrombotic risk factors.
Design/Methods: We used a multicenter, retrospective cohort study of the Virtual Pediatric Systems database including 141 pediatric intensive care units from Jan 2014 - Dec 2023 to assess those aged 0-21 years with a primary diagnosis of DKA. We excluded neonatal encounters, those following cardiothoracic surgery, and for a length of stay (LOS) < 1 day. The primary aim was to estimate the frequency rate of HA-VTE. Area under the receiver operator characteristic (AUROC) curve analyses was used to discriminate DKA-related prothrombotic risk factors. Unadjusted and adjusted logistic regression were employed to assess putative HA-VTE risk factors.
Results: Of 21,549 encounters studied, 62 (0.29%) developed HA-VTE. Compared to those without HA-VTE, those with experienced greater rates of sepsis (43.5% vs 0.7%), cerebral edema (17.7% vs 3.1%), central venous catheterization (CVC, 66.2% versus 3.8%), invasive mechanical ventilation (IMV, 46.8% vs 2.3%) elevated LOS (median 4.9 [interquartile range{IQR}: 2.6-12.2] vs 1.4 [IQR: 1.1-1.9] days), acidosis (median pH: 6.96 [IQR: 6.82-7.13] vs 7.07 [IQR: 6.96-7.18]; bicarbonate 5 [IQR: 5-9] vs 6 [IQR: 5-10] mmol/L), hyperglycemia (median 590 [IQR: 453-802] vs 406 [IQR: 310-548] mg/dL) and reduced Glasgow Coma Scores (median 12 [IQR: 6-14] vs 15 [IQR: 14-15]) (all p< 0.001) (Figure 1). AUROC for pH, bicarbonate, glucose, and GCS were 64.8% (95% CI: 55.5% - 74.1%), 53.5% (95% CI: 45.9% – 61.1%), 72.2% (95% CI: 65.6 - 78.8%), and 75.5% (95% CI: 66.1%-84.9%), respectively (Figure 2). Factors associated with HA-VTE were CVC (adjusted odds ratio [aOR]: 15.43, 95% confidence interval [CI]: 3.92-60.68, p< 0.001), sepsis (aOR: 5.08, 95%CI: 1.78-14.5, p=0.002), and LOS ≥4 days (aOR: 4.19, 95%CI: 1.26-14.01, p=0.02). No DKA-related clinical features were associated with HA-VTE.
Conclusion(s): In this multicenter observational study the estimated occurrence rate of HA-VTE among critically ill children and young adults was 0.29%. While hyperglycemia and acidosis may be discriminatory for HA-VTE, only CVC, concurrent infection, and extended LOS were associated with HA-VTE.
Letter from Graduate Medical Education Office containing dates of house officer training
GME Letter of Training Dates.pdf
Figure 2
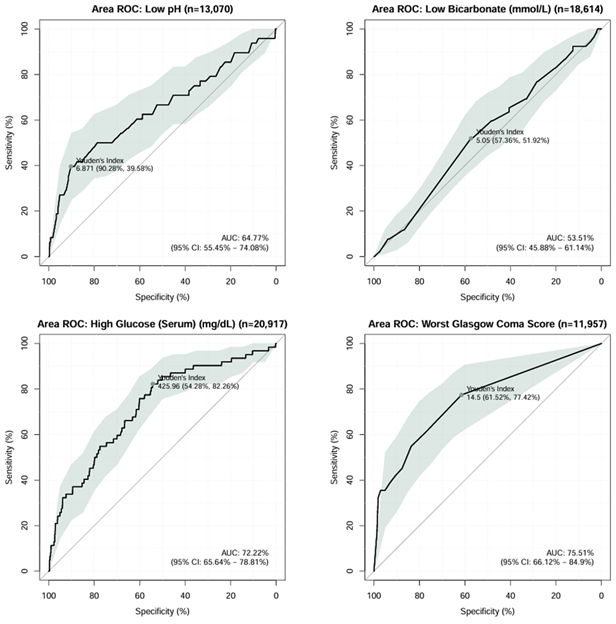 Receiver operator characteristic curve analyses for lowest pH, bicarbonate, Glasgow Coma Scale, and serum glucose within 24-hours of admission among critically ill children and young adults with diabetic ketoacidosis reporting area under the curve with 95% confidence interval, Youden’s index threshold value, and accompanying sensitivity and specific values.
Receiver operator characteristic curve analyses for lowest pH, bicarbonate, Glasgow Coma Scale, and serum glucose within 24-hours of admission among critically ill children and young adults with diabetic ketoacidosis reporting area under the curve with 95% confidence interval, Youden’s index threshold value, and accompanying sensitivity and specific values.
