Mental Health 3
Session: Mental Health 3
077 - Determining the Impact of Ethno-Racial Trauma on the Well-being of U.S. Physicians and Physician Trainees: A Scoping Review
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 77.4220
Uchechi Oddiri, Renaissance School of Medicine at Stony Brook University, Stony Brook, NY, United States; Rakasa Pattanaik, Renaissance School of Medicine at Stony Brook University, East Setauket, NY, United States; Adam Cohen, Baylor College of Medicine/Texas Children's Hospital, Houston, TX, United States; Mary L. Ehlenbach, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States; Kajal Khanna, Stanford University School of Medicine, San Francisco, CA, United States; Heidi Kloster, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States; Laurel Scheinfeld, Stony Brook University - Health Sciences Library, Stony Brook, NY, United States
Uchechi Oddiri, MD, FAAP (she/her/hers)
Clinical Assistant Professor of Pediatrics
Renaissance School of Medicine at Stony Brook University
Stony Brook, New York, United States
Presenting Author(s)
Background: Racism serves as a source of stress for providers. Underrepresented in medicine physicians and trainees are disproportionately susceptible to the trauma stemming from systemic inequities, resulting in discrimination, limited career advancement, leadership opportunities, mentorship, and representation. There is a need to investigate the impact of systemic racism on provider wellbeing.
Objective: This review aims to map existing literature to determine the impact ethno-racial trauma (ERT), defined as the psycho-emotional injury caused by the mistreatment or discrimination of a person based on their race or ethnicity, experienced by physicians and physician trainees (resident/fellow physicians or medical students) has on their wellbeing.
Design/Methods: This scoping review was conducted according to JBI methodology. A comprehensive search strategy was created with an information specialist and underwent peer review. The search was performed in 6 bibliographic databases and 1 grey literature source with no timeframe restriction. All English language studies conducted in the US that assessed the impact of ERT on physicians and physician trainees were included. Study selection involved a title/abstract screening followed by fulltext review. Three pairs of reviewers screened results and extracted data.
Results: Out of 4656 studies identified for initial screening, 534 studies underwent full-text review, and 94 studies met inclusion criteria, with 29 studies focused on physicians alone, 47 focused on physician trainees alone, and 18 focused on both (Fig. 1). Included studies were published between 1987 and 2024 (Fig. 2). Study designs included observational, qualitative, mixed methods, and reviews (Fig. 3). The most frequently reported forms of ERT experienced by providers included discrimination, microaggressions, isolation or feeling invisible, and implicit bias. Patients, community members, faculty and preceptors, residents, peers, and other practitioners were identified as sources of ERT. ERT sustained by both physicians and physician trainees was often associated with burnout, isolation, and stress. This ERT had a negative impact on elements of wellbeing, most notably the emotions, learning experience, mental health, and confidence for physician trainees, and the career advancement and satisfaction, emotions, accomplishment, and confidence for physicians.
Conclusion(s): Existing literature regarding ERT experienced by medical providers demonstrate its impact on their wellbeing. There is need for prospective interventional studies to evaluate the effects of ERT and strategically mitigate its impact on wellbeing.
Figure 1: PRISMA Flow Diagram
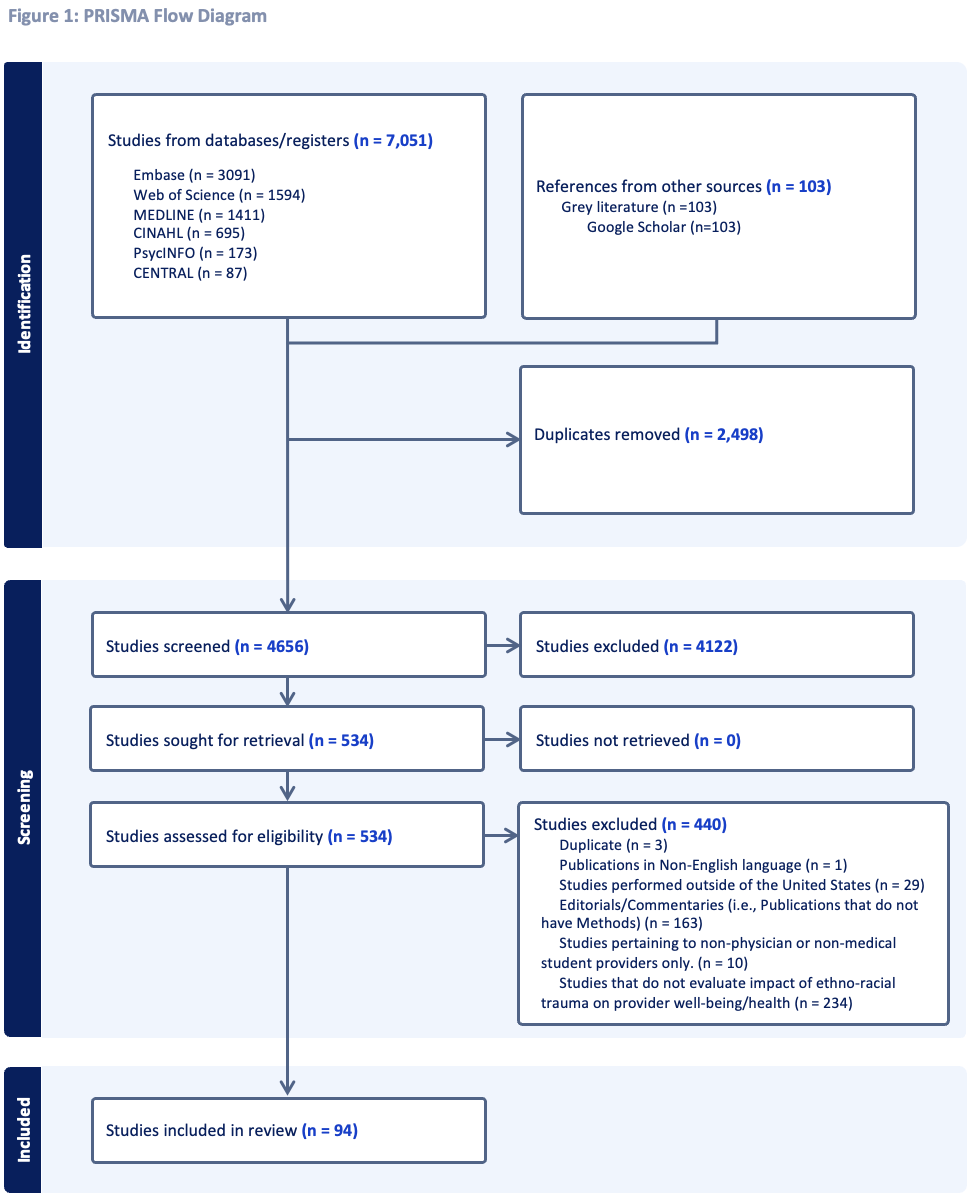 This PRISMA Flow Diagram depicts the screening and article selection process used in this scoping review.
This PRISMA Flow Diagram depicts the screening and article selection process used in this scoping review.Figure 2: Number of Studies per Year
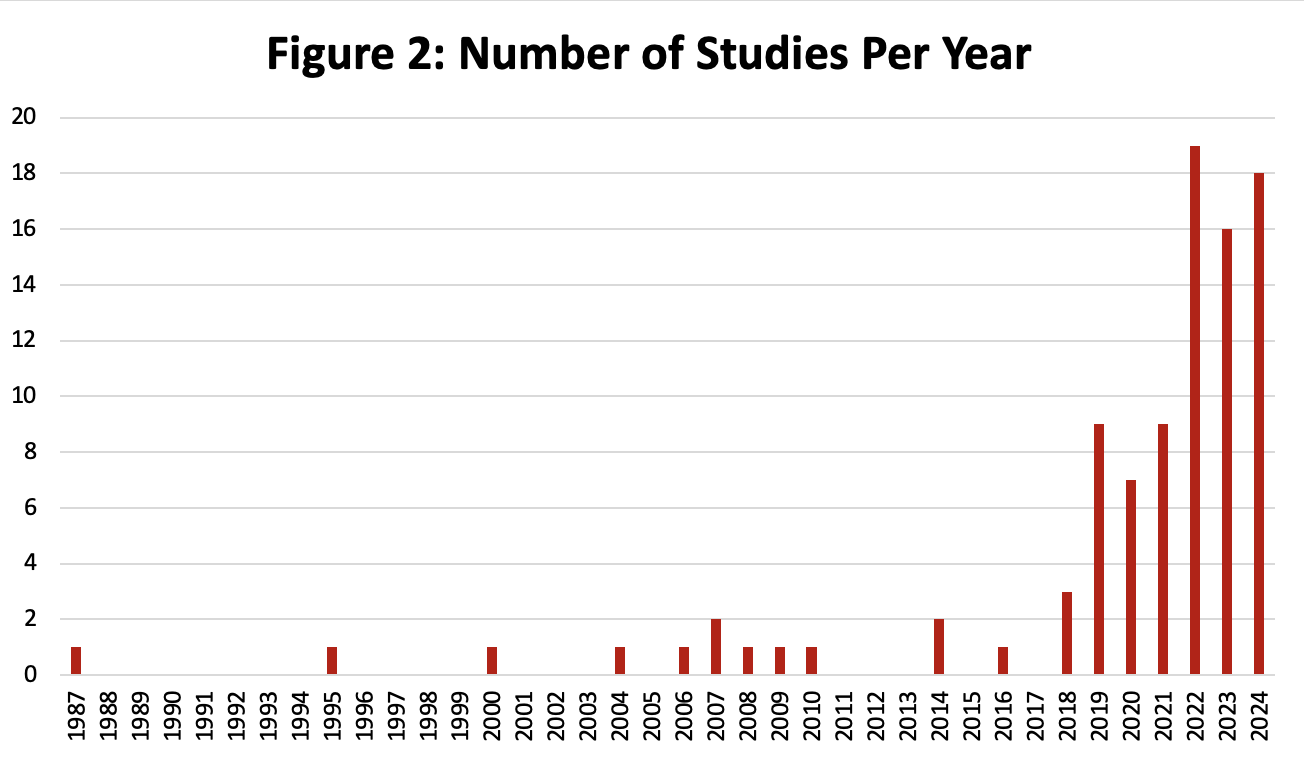 This graph depicts the distribution of included articles by the year of publication.
This graph depicts the distribution of included articles by the year of publication.Figure 3: Study Designs
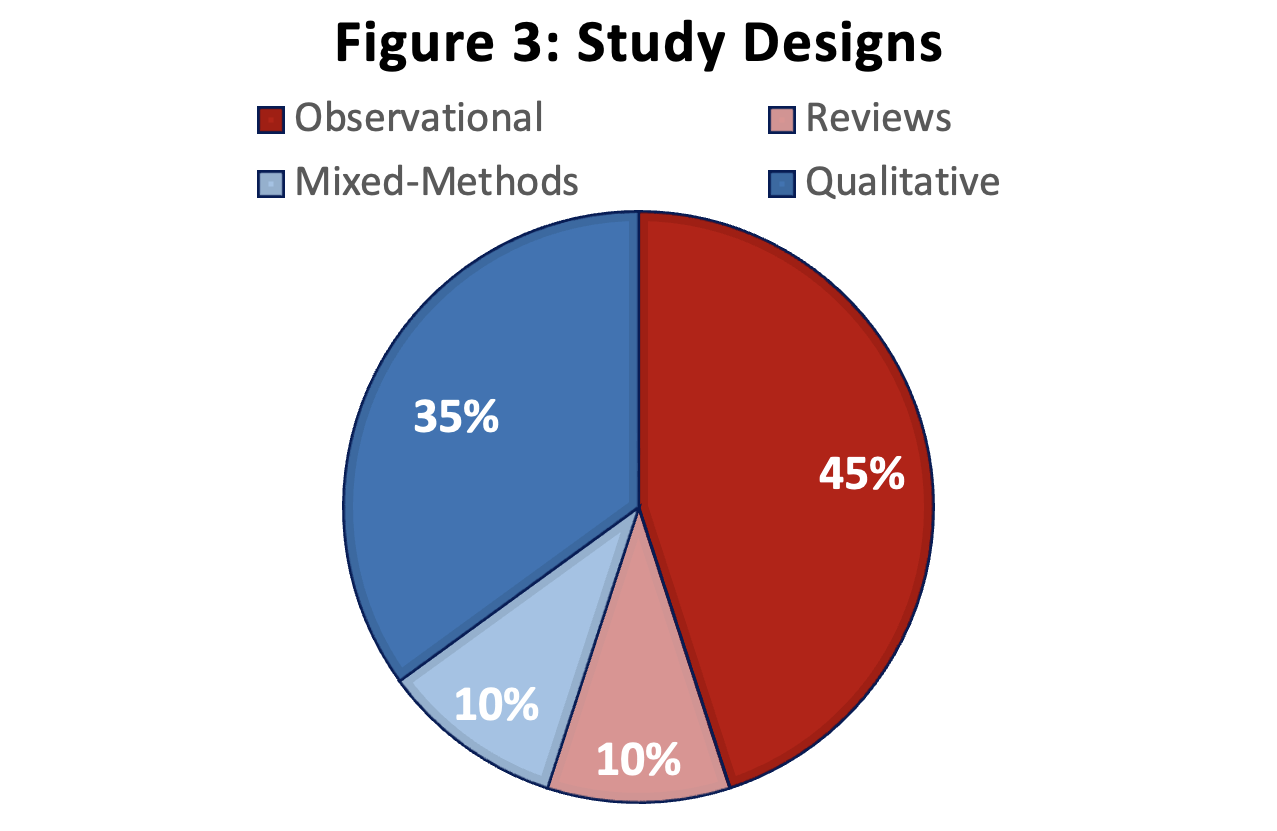 This chart depicts the study designs of included articles in this scoping review.
This chart depicts the study designs of included articles in this scoping review.
